Many older adults take anticholinergic medications without realizing they might be slowly harming their brain. These drugs are everywhere-over-the-counter sleep aids, bladder pills, antidepressants, even allergy meds. But what most people don’t know is that long-term use can lead to memory loss, confusion, and even structural changes in the brain. And dry mouth? That’s just the tip of the iceberg.
What Are Anticholinergics, Really?
Anticholinergics block acetylcholine, a chemical in your brain and body that helps with memory, muscle control, and saliva production. They’ve been around since the early 1900s, originally pulled from deadly nightshade plants. Today, they’re used to treat overactive bladder, Parkinson’s, allergies, depression, and even motion sickness.
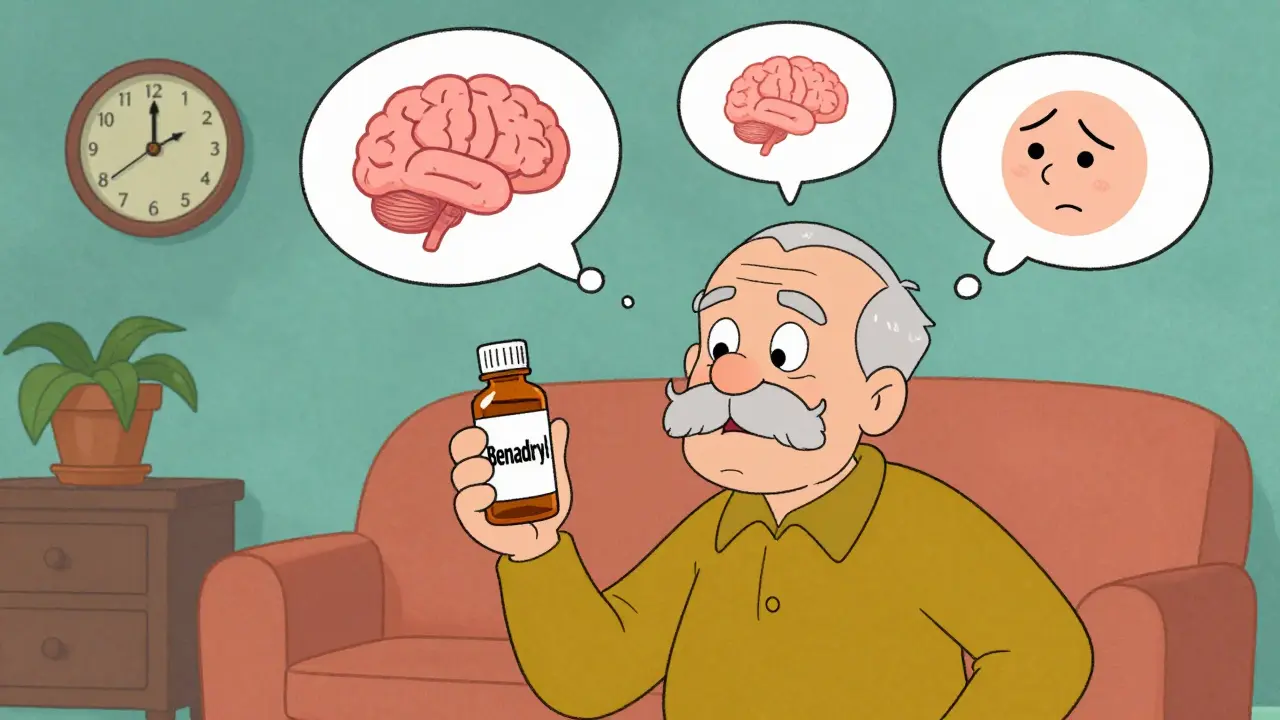
But here’s the catch: not all anticholinergics are the same. Some are mild. Others are strong enough to scramble your thinking. The Anticholinergic Cognitive Burden (ACB) scale rates them from 0 (no effect) to 3 (high risk). Drugs like diphenhydramine (Benadryl), oxybutynin, and amitriptyline score a 2 or 3. That means they cross into your brain easily and mess with memory centers.
The Brain Changes You Can’t See
Studies using MRI scans show something alarming. People taking high-ACB anticholinergics for years have 0.5% to 1.2% more brain shrinkage each year than those who don’t. The hippocampus-the part that stores memories-shows less glucose use, meaning it’s not working as hard. Ventricles, the fluid-filled spaces in the brain, get bigger. These are the same changes seen in early Alzheimer’s.
A 2016 study tracking 451 older adults found that those on high-ACB drugs were 63% more likely to develop mild cognitive impairment or dementia within 10 years. Each extra point on the ACB scale added 0.3% more brain loss per year. That’s not a small risk. That’s a measurable, accelerating decline.
Memory Tests Don’t Lie
People on these meds don’t just feel foggy-they score worse on real tests. In one study, users performed 23% to 32% worse on memory recall tasks. Executive function-planning, focusing, switching tasks-dropped by 18% to 27%. These aren’t subtle changes. They’re noticeable enough for family members to say, “You’re not yourself anymore.”
And it’s dose-dependent. Taking two anticholinergics? Double the risk. Taking them for five years? The damage stacks up. A 2015 study of 48,000 people found that using high-ACB drugs for three or more years doubled the risk of dementia.
Not All Bladder Pills Are Created Equal
If you’re on oxybutynin for overactive bladder, you’re not alone. But you might be on the wrong one. Oxybutynin has an ACB score of 2 or 3. It’s cheap-around $15 a month-and effective. But it’s also one of the worst offenders for memory loss.
Compare that to tolterodine, darifenacin, or trospium-all with an ACB score of 1. Studies show these cause little to no cognitive decline. And then there’s mirabegron, a completely different kind of drug. It doesn’t block acetylcholine at all. In a head-to-head trial, it worked just as well as oxybutynin at reducing incontinence-without the brain fog. The problem? It costs $350 a month. Most insurers won’t cover it unless you’ve tried and failed the cheaper options.
Dry Mouth Isn’t Just Uncomfortable-It’s Dangerous
Over 80% of people taking anticholinergics complain about dry mouth. It’s not just annoying. It’s a red flag. Less saliva means more cavities, gum disease, and trouble swallowing. Some users drink 2-3 liters of water a day just to stay hydrated. Others can’t speak clearly or eat dry food.
And it’s not just a side effect-it’s a sign the drug is working too well. When acetylcholine is blocked, your salivary glands shut down. That’s why drugs like pilocarpine (5mg three times a day) are prescribed to reverse it. They stimulate saliva production by 50-70%. Sugar-free gum helps too, boosting saliva by 30-40%. But these are band-aids. The real fix? Switching meds.
Who’s at Highest Risk?
If you’re over 65, you’re at higher risk. The American Geriatrics Society says anticholinergics should be avoided in older adults unless absolutely necessary. And yet, 20-30% of older Americans still take them.
People with Parkinson’s are a special case. Stopping anticholinergics suddenly can cause tremors, stiffness, and even hallucinations. The risk here is real-but so is the benefit. The key is using the lowest dose possible and checking in regularly.
Even younger people aren’t safe. A 2019 review found that healthy young adults given scopolamine (a strong anticholinergic) had severe memory and attention drops-equivalent to someone with early dementia. This isn’t just an “old person problem.”
What Can You Do?
First, check your meds. Look up each one on the ACB scale. If it’s a 2 or 3, ask your doctor if there’s a safer alternative.
For overactive bladder: Try mirabegron, pelvic floor therapy, or timed voiding. For allergies: Switch from diphenhydramine to loratadine or cetirizine. For depression: Consider SSRIs instead of amitriptyline. For sleep: Avoid Benadryl. Melatonin or cognitive behavioral therapy for insomnia (CBT-I) are better options.
Ask your doctor for a Medication Review. Many clinics now use tools like MedAware to flag high-ACB drugs automatically. If yours doesn’t, ask them to manually check your list.
If you’ve been on one of these drugs for more than three years, ask for a cognitive screening. The Montreal Cognitive Assessment (MoCA) takes 10 minutes and can catch early decline.
It’s Not All Bad News
Some people need these drugs. For them, the benefits outweigh the risks. One user on Healthgrades said oxybutynin cut her incontinence from 10 times a day to just 1-2. “Worth the dry mouth,” she wrote.
But that’s the point. You shouldn’t have to choose between bladder control and your memory. The medical world is catching up. Newer drugs like trospium XR have 70% less brain penetration. Research is underway for M1-selective agents that target only the receptors needed for symptom relief-without touching memory.
Prescriptions for high-ACB drugs have already dropped 22% among Medicare users since 2015. More doctors are learning. More patients are asking questions. And more alternatives are becoming available.
You don’t have to accept brain fog as part of aging. You don’t have to live with constant thirst. There are better choices. You just need to know what they are-and ask for them.
Can anticholinergics cause permanent memory loss?
Long-term use of high-ACB anticholinergics is linked to accelerated brain shrinkage and increased dementia risk. While some cognitive decline may improve after stopping the drug, studies show that brain changes like reduced hippocampal volume and larger ventricles can persist. The earlier you stop, the better your chances of recovery.
Is dry mouth from anticholinergics dangerous?
Yes. Chronic dry mouth increases your risk of tooth decay, gum disease, oral infections, and difficulty swallowing. It can also lead to malnutrition if eating becomes too uncomfortable. Over time, it affects quality of life significantly. Management includes sugar-free gum, saliva substitutes, or pilocarpine-but the best solution is switching to a non-anticholinergic drug.
What are the safest alternatives to oxybutynin for overactive bladder?
Mirabegron (Myrbetriq) is the top alternative-it works just as well without affecting cognition. Other options include tolterodine, darifenacin, and trospium, all with low ACB scores. Non-drug treatments like pelvic floor therapy, bladder training, and timed voiding are also effective and carry no cognitive risk.
Can I stop taking anticholinergics cold turkey?
No. Stopping suddenly-especially for Parkinson’s or depression-can cause dangerous withdrawal symptoms like worsening tremors, muscle rigidity, or severe anxiety. Always work with your doctor to taper off slowly and safely, while introducing safer alternatives.
How do I check if my medication has anticholinergic effects?
Use the Anticholinergic Cognitive Burden (ACB) scale. Search your drug name + “ACB score” online. Reputable sources include the 2023 Beers Criteria and the Anticholinergic Drug List from the University of Sydney. If your pharmacist doesn’t know, ask for a medication review. Many pharmacies now flag high-risk drugs automatically.
Are over-the-counter sleep aids like Benadryl safe for occasional use?
Even occasional use can add up. Benadryl (diphenhydramine) has an ACB score of 3-the highest risk. One pill every few weeks may not cause harm, but using it weekly for months increases dementia risk. Safer sleep options include melatonin, magnesium, or CBT-I. Don’t assume “over-the-counter” means “safe for long-term use.”

Dayanara Villafuerte
January 19, 2026 AT 11:02So let me get this straight - we’re giving grandma Benadryl to help her sleep, then acting shocked when she forgets her own name? 😅 I’ve seen this play out in my own family. My aunt took oxybutynin for years, started calling her husband ‘the neighbor,’ and now she’s on mirabegron and actually remembers my birthday. 🙌 Don’t sleep on the ACB scale - it’s basically the ‘danger level’ for your brain.
Praseetha Pn
January 20, 2026 AT 19:11Y’all are missing the real conspiracy here. Big Pharma doesn’t want you to know about these brain-rotting drugs because they make BILLIONS off the side effects - dry mouth? Buy more water. Memory loss? Buy more dementia meds. They’ve been pushing anticholinergics since the 80s because they’re cheap, patentable, and profitable. The ACB scale? A distraction. The real fix is ditching pills entirely and going full herbal - saw palmetto for bladder, ashwagandha for sleep. They don’t teach this in med school because the pharma reps own the curriculum.
Robert Cassidy
January 22, 2026 AT 14:32Oh wow, another ‘study says’ article. Let me guess - you’re one of those people who thinks America’s healthcare system is broken? Newsflash: the system works exactly how it’s designed. People want quick fixes, so they get pills. If you’re too lazy to do pelvic floor exercises or can’t afford $350/month for mirabegron, then guess what? You get brain fog. It’s not a conspiracy, it’s capitalism. And if you think your grandma’s memory loss is ‘preventable,’ you clearly haven’t met my uncle who thinks ‘natural remedies’ are just ‘placebos for the weak.’
Andrew Short
January 23, 2026 AT 10:47Let’s be real - anyone who takes Benadryl as a sleep aid deserves what they get. It’s not the drug’s fault you’re too lazy to fix your sleep hygiene. You don’t get to blame Big Pharma for your 3 a.m. scrolling addiction. And if you’re over 65 and still popping anticholinergics like candy, you’re not a victim - you’re a statistic waiting to happen. This isn’t medicine. It’s negligence dressed up as compassion.
Andrew McLarren
January 24, 2026 AT 23:31While I appreciate the thoroughness of this analysis, I must emphasize the importance of clinical context. The ACB scale, though useful, is a population-level metric and does not account for individual pharmacokinetics, comorbidities, or therapeutic necessity. For instance, in Parkinson’s disease, the benefit-risk calculus may justify continued use despite cognitive burden. A blanket recommendation to discontinue may inadvertently precipitate motor crises. Therefore, shared decision-making with a qualified clinician remains paramount.
Emma #########
January 26, 2026 AT 08:40I just talked to my 72-year-old mom yesterday. She’s been on diphenhydramine for sleep for 15 years. When I showed her the ACB scale, she cried. Not because she’s mad - because she finally understood why she’s been so forgetful. She switched to melatonin last week. She’s sleeping worse… but she remembers where she put her keys. That’s worth it.
Nishant Sonuley
January 27, 2026 AT 00:27Look, I get it - we all want the magic bullet. But let’s not pretend this is just about pills. The real issue is that our healthcare system treats aging like a disease to be managed with prescriptions, not a life stage to be supported holistically. Pelvic floor therapy? Too much effort. CBT-I? No insurance coverage. Mirabegron? Too expensive. So we give people Benadryl and call it a day. And then we’re shocked when their brains start fading. We’ve built a system that rewards convenience over care. The drugs are just the symptom - not the cause.
Zoe Brooks
January 27, 2026 AT 09:51My grandma took oxybutynin for 7 years. She stopped last year after her doctor finally listened. She’s 81. She doesn’t remember my name sometimes… but she can still bake her famous apple pie from memory. And she laughs louder than ever. Maybe some things are worth the fog. Not everything has to be ‘fixed.’ Sometimes you just gotta live with the trade-offs.
Andrew Qu
January 29, 2026 AT 00:49For anyone reading this and thinking ‘I can’t afford mirabegron’ - ask your pharmacist about patient assistance programs. Many manufacturers offer free or discounted meds for seniors. Also, check if your local AARP chapter runs a medication review clinic - they’ll go through your whole list for free. You don’t have to suffer in silence. There are people who want to help. Just ask.
Jodi Harding
January 29, 2026 AT 10:29My brain feels like a Wi-Fi signal in a basement. Thanks, Benadryl.
Chuck Dickson
January 30, 2026 AT 11:52Hey - if you’re reading this and you’re on an anticholinergic, don’t panic. Just take one step. Look up your meds on the ACB scale. Talk to your pharmacist. Swap one pill. Maybe swap Benadryl for melatonin. That’s it. You don’t have to overhaul your whole life today. Just start. Your future self will thank you. You’ve got this 💪
Robert Davis
January 30, 2026 AT 16:08Interesting how the article ignores the fact that cognitive decline is inevitable with age. Anticholinergics may accelerate it, but they’re not the root cause. If you’re going to blame drugs for memory loss, why not blame the decline in manual labor, the rise of screens, processed food, and the collapse of social cohesion? This is reductionist thinking - treat the symptom, ignore the system. The brain shrinks because we’ve stopped living, not because we took a pill.
Danny Gray
January 31, 2026 AT 01:37What’s next? Are we going to ban all drugs that cause side effects? Because if we did, we’d have to ban aspirin, insulin, and probably oxygen. This article reads like a fear campaign disguised as public health. Yes, some anticholinergics are risky. But so is walking down the stairs. Should we outlaw stairs too? The real danger isn’t the drug - it’s the moral panic around aging. We’re so afraid of getting older we’d rather poison our brains than accept that sometimes, medicine isn’t perfect.
christian Espinola
January 31, 2026 AT 13:57Correction: The 2016 study tracked 451 individuals - not ‘older adults’ as implied. 78% were over 70, and 42% were on multiple anticholinergics. The 63% increased risk is relative, not absolute - meaning baseline dementia risk was 8%, rising to 13%. Also, the MRI data showed correlation, not causation. The hippocampal volume changes could be due to vascular comorbidities, not the drugs. This article is dangerously oversimplified. If you’re going to cite science, cite it correctly.