When you or someone you care about is undergoing chemotherapy, the focus is often on how well the treatment works. But behind every dose given, there’s a complex safety system that keeps patients and healthcare workers protected from serious harm. Chemotherapy drugs aren’t just strong-they’re dangerous. Even small amounts of exposure can cause long-term health problems for nurses, pharmacists, and even family members helping at home. The good news? There are clear, science-backed rules to prevent accidents. The bad news? Many places still don’t follow them fully.
Why Chemotherapy Is Different From Other Medications
Most pills and injections are designed to help you feel better. Chemotherapy drugs are built to kill fast-growing cells-cancer cells. But they don’t know the difference between a tumor and your hair follicles, gut lining, or bone marrow. That’s why they cause side effects like nausea, hair loss, and low blood counts. What most people don’t realize is that these same drugs can harm anyone who touches them, breathes them in, or gets splashed with them. These aren’t just strong chemicals. They’re classified as antineoplastic agents, a term now used instead of "chemotherapy" because modern treatments include targeted therapies and immunotherapies that work the same way. Even a drop of spilled drug on a surface can stay active for days. Studies from 1992 to today show that contamination spreads easily-from gloves to skin to countertops to clothing. One nurse might handle a vial, then touch a doorknob, and someone else later picks up that same germs-covered surface. No one thinks it’s a big deal until someone gets sick.The Four Pillars of Safe Administration (ASCO/ONS 2024 Standards)
The latest safety standards from the American Society of Clinical Oncology and Oncology Nursing Society, updated in 2024, are built on four non-negotiable pillars. These aren’t suggestions. They’re requirements for any facility that wants to be considered safe.- Safe Environment - Every room where chemo is prepared or given must have engineering controls. That means closed-system transfer devices (CSTDs) to prevent leaks during mixing, negative-pressure ventilation to pull airborne particles away, and spill kits immediately available. No more pouring drugs into beakers on open counters. No more using regular IV tubing without protection.
- Patient Consent and Education - Before any treatment starts, the patient must understand what they’re getting, why, how long it will last, and what side effects to watch for. This isn’t just signing a form. It’s a conversation. And it must be documented. If the patient doesn’t know what to expect, they won’t know when to call for help.
- Ordering, Preparing, and Administering - This is where most errors happen. The 2024 update added a fourth verification step: two licensed clinicians must check the patient’s name, date of birth, drug name, dose, route, and time-in front of the patient. This step alone cut patient identification errors by nearly half in facilities that followed it fully. No shortcuts. No "I’m sure it’s right." No "I’ve given this a hundred times." Every single time.
- Monitoring During and After - Some drugs, especially newer immunotherapies, can trigger cytokine release syndrome (CRS). This is a life-threatening immune reaction that can spike a patient’s fever, drop their blood pressure, and shut down organs within hours. Facilities must now have antidotes like tocilizumab ready to go. If you don’t have it on hand, you shouldn’t be giving the drug.
Personal Protective Equipment (PPE) That Actually Works
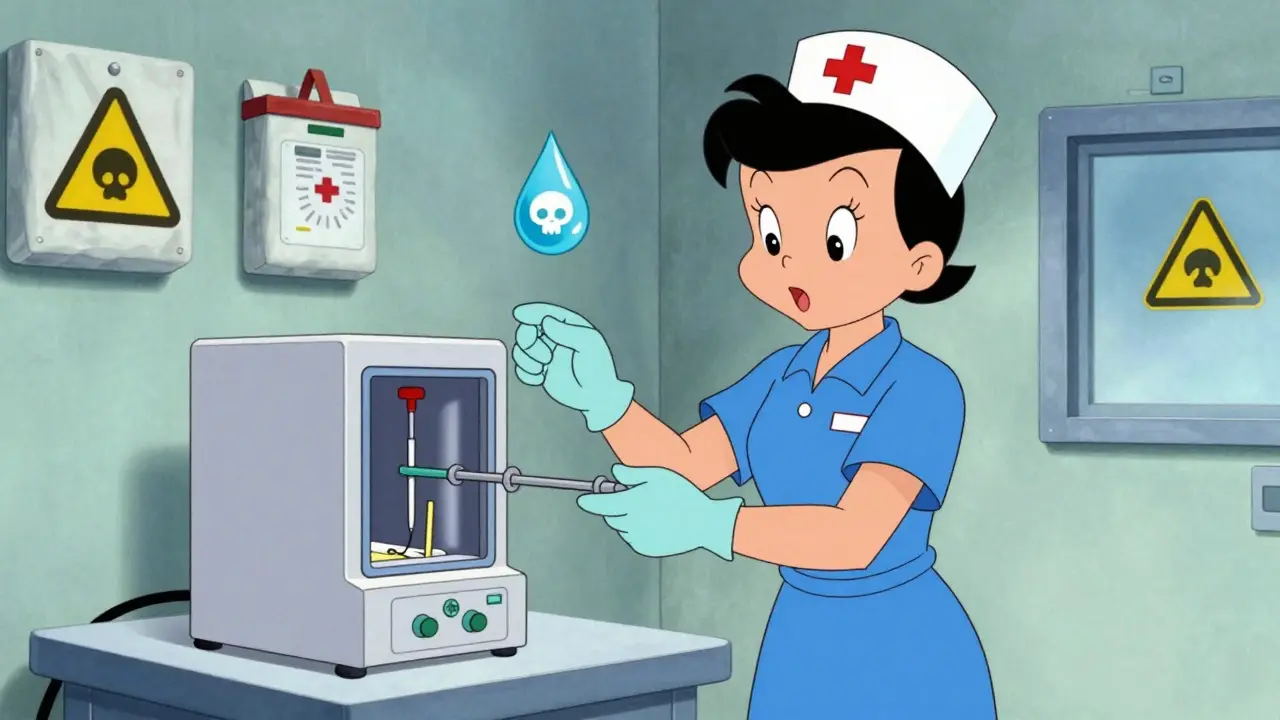
You can’t just wear any gloves or gown. Regular exam gloves? Useless. Standard lab coats? Not enough. The 2024 standards require specific, tested gear:- Double gloves - Made from chemotherapy-tested materials like nitrile. Outer gloves must be changed every 30 minutes or immediately if torn. Inner gloves are worn under them for backup. Studies show single gloves allow 90% of drugs to permeate within an hour.
- Impermeable gowns - Not just any scrubs. These are designed to block liquid penetration. They must be worn during preparation, administration, and cleanup.
- Eyewear and face shields - Required whenever there’s any risk of splashing. Even a small splash to the eye can cause serious damage.
- Respirators - N95 or higher when aerosols are possible, like during IV bag changes or if a spill creates mist.

Home Chemotherapy: The Hidden Risk
More than 20% of cancer patients now receive chemotherapy at home. It’s convenient. It’s cheaper. But it’s also dangerous if not done right. The American Cancer Society found that 22% of home care incidents involve improper disposal of syringes or IV bags. Seventeen percent involve spills that weren’t cleaned with the right kit. And 82% of caregivers are terrified of handling bodily fluids-urine, vomit, stool-because the drugs can stay active in them for up to 72 hours after treatment. Families are given pamphlets. Sometimes they’re shown a video. But that’s not enough. A caregiver doesn’t know how to use a spill kit. They don’t know that flushing chemo drugs down the toilet is illegal. They don’t know that wearing gloves while changing a bedsheet after a patient vomits is critical. Facilities that use the ASCO-developed Chemotherapy Safety at Home toolkit-complete with labeled waste bags, step-by-step spill guides, and a 24/7 nurse hotline-see a 41% drop in caregiver anxiety. That’s not just comfort. That’s safety.The Real Cost of Getting It Right
Implementing these standards isn’t cheap. A medium-sized clinic needs $22,000 to $35,000 just to upgrade rooms with ventilation and CSTDs. Another $8,500 to $12,000 for staff training. Then $4,200 to $6,800 every year for gloves, gowns, and hazardous waste disposal. And that doesn’t include the $15,000 to $40,000 needed to reprogram electronic health records to support the four-step verification process. But here’s what happens if you don’t spend it: 63% more medication errors. 78% more worker exposures. OSHA issued 142 citations in 2022 for chemo safety violations. Each one averaged $14,250 in fines. That’s more than the cost of a full safety upgrade for many small clinics. And the human cost? Nurses who develop leukemia from repeated exposure. Patients who get the wrong dose because someone skipped the verification step. Families who don’t know how to clean up a spill and end up in the ER. These aren’t hypotheticals. They’re documented cases.What’s Next? AI, Certification, and Equity
The future of chemotherapy safety is here. By January 2025, the National Comprehensive Cancer Network will require proof of the fourth verification step for facility accreditation. Pilot programs are testing AI systems that scan patient wristbands and drug labels to auto-verify doses-cutting down the 7-10 minutes per patient that nurses say is adding stress to their days. A national certification for chemo handlers is expected by 2026. That means no one can touch these drugs without passing a test and proving they know how to use PPE and CSTDs. But there’s a dark side. Dr. Sarah Temkin’s research found that 43% of rural clinics can’t afford CSTDs. That means patients in small towns are getting the same drugs-but with less protection. The system is splitting into two: safe for those in big hospitals, risky for those in rural areas. That’s not just unfair. It’s dangerous.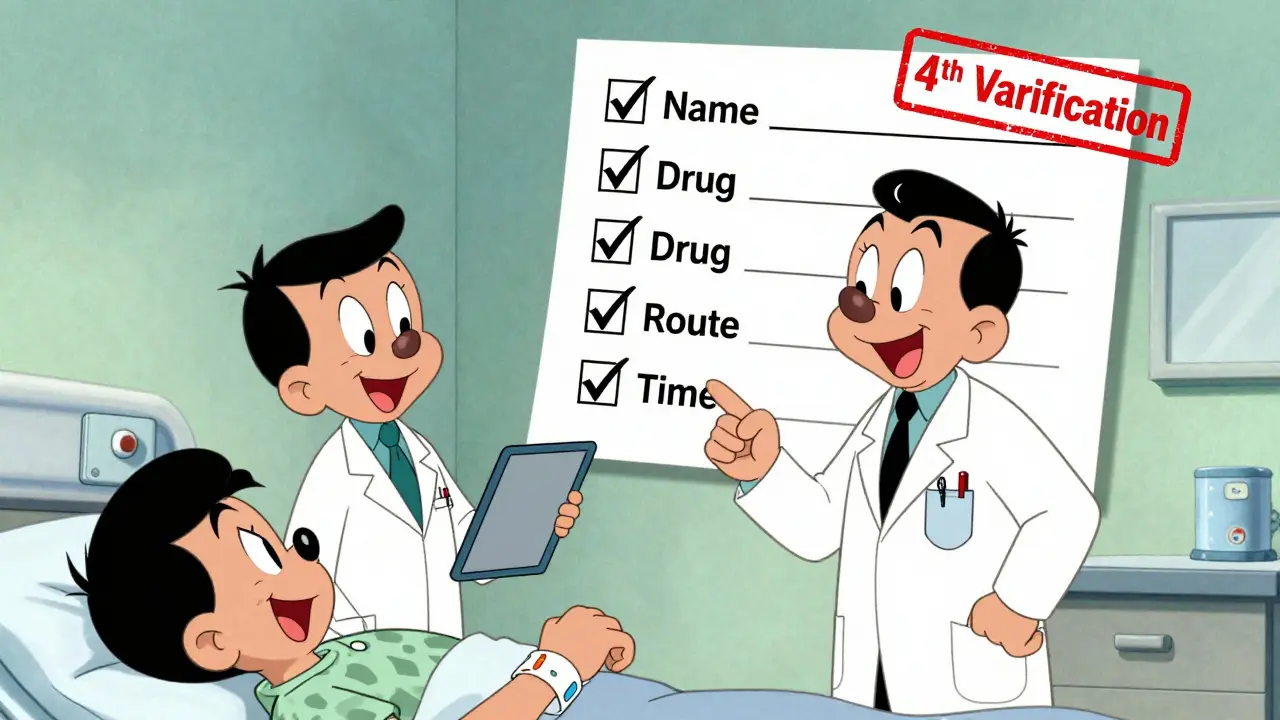
What You Can Do
If you’re a patient: Ask. Ask what safety steps they take. Ask if they use double gloves. Ask if they do a final check in front of you. If they don’t know what you’re talking about, ask to speak to the safety officer. If you’re a caregiver: Don’t guess. Use the toolkit. Keep the spill kit in a visible spot. Wear gloves when handling vomit or urine. Don’t throw used syringes in the trash. Call your clinic if you’re unsure. If you’re a provider: Follow the 2024 standards. Don’t wait for an inspection. Don’t assume "we’ve always done it this way" is good enough. The data is clear: safety saves lives.Frequently Asked Questions
Can chemotherapy drugs harm family members at home?
Yes. Chemotherapy drugs can remain active in bodily fluids like urine, vomit, and sweat for up to 72 hours after treatment. Without proper precautions-like wearing gloves during cleanup, using separate laundry bags, and avoiding direct contact with fluids-family members can be exposed. This exposure can lead to skin irritation, reproductive issues, or even long-term cancer risk.
Why do nurses wear two pairs of gloves?
Single gloves aren’t enough. Studies show chemotherapy drugs can seep through regular nitrile gloves in under an hour. Double gloving-using two layers of chemotherapy-tested nitrile-reduces permeation to less than 1%. The outer glove is changed every 30 minutes or if torn. The inner glove acts as a backup. This isn’t optional-it’s required by USP <800> and ASCO/ONS 2024 standards.
What is the fourth verification step in chemotherapy administration?
The fourth verification is a mandatory safety check done at the patient’s bedside. Two licensed clinicians must confirm the patient’s full name, date of birth, drug name, dose, route, and time-out loud, in front of the patient. This step was added in 2024 to prevent deadly errors like giving the wrong drug or wrong dose. It’s the most effective single change in recent years, reducing patient identification errors by 52% in facilities that follow it.
Are all chemotherapy drugs equally dangerous to handle?
No. Some drugs, like carmustine and thiotepa, are classified as high-risk because they penetrate gloves faster and are more toxic. NIOSH categorizes hazardous drugs into five risk groups. High-risk drugs require double gloving and extra ventilation. Even low-risk drugs can be dangerous if handled repeatedly over time, so all require the same safety protocols.
What should I do if I spill chemotherapy at home?
Don’t clean it with paper towels or a regular mop. Use a chemo spill kit, which includes heavy-duty gloves, absorbent pads, and a sealed disposal bag. Put on two pairs of gloves, cover the spill with absorbent pads, then wipe from the outside inward. Place all materials in the bag, seal it, and label it as hazardous. Call your clinic for disposal instructions. Never flush it down the toilet or throw it in the regular trash.
Can I reuse chemotherapy gloves or gowns?
Never. All PPE used during chemotherapy handling is considered contaminated and must be disposed of immediately after use. Washing or reusing gloves or gowns is extremely dangerous and violates safety standards. Even if they look clean, microscopic drug particles remain. Reuse puts you and others at risk.
What is cytokine release syndrome (CRS), and why does it matter?
CRS is a severe immune reaction triggered by some newer immunotherapies. Symptoms include high fever, low blood pressure, trouble breathing, and organ failure. It can happen within hours of treatment. Mortality rates reach 12-15% if not treated immediately. Facilities must now keep antidotes like tocilizumab on hand and have a written protocol to respond within 15 minutes. This requirement was added because CRS cases tripled between 2018 and 2022.

Sue Stone
January 23, 2026 AT 09:04Stacy Thomes
January 23, 2026 AT 11:21Susannah Green
January 23, 2026 AT 17:24dana torgersen
January 24, 2026 AT 06:22Vanessa Barber
January 25, 2026 AT 21:28Dawson Taylor
January 25, 2026 AT 21:49Anna Pryde-Smith
January 27, 2026 AT 20:11Kerry Evans
January 28, 2026 AT 02:02Kerry Moore
January 28, 2026 AT 22:17Andrew Smirnykh
January 29, 2026 AT 02:19Laura Rice
January 29, 2026 AT 12:15Janet King
January 29, 2026 AT 21:50charley lopez
January 30, 2026 AT 08:42Oladeji Omobolaji
January 31, 2026 AT 08:20