When a life-saving drug runs out, hospitals don’t just wait for more to arrive. In the U.S., the FDA steps in with a quiet but powerful tool: extended expiration dates. This isn’t about stretching out old medicine for convenience. It’s a carefully controlled, science-backed move to keep patients alive when supply chains break down.
Why Extended Expiration Dates Exist
Drug shortages aren’t rare. They happen because of manufacturing delays, quality issues, or single-source production. One factory goes offline, and suddenly hospitals can’t get propofol for surgery, epinephrine for allergic reactions, or IV fluids for dehydration. The FDA doesn’t have the power to force companies to make more. But it can do something else: let providers use drugs past their printed expiration date-if the data says it’s safe. This isn’t new. The legal authority came from the Food and Drug Administration Safety and Innovation Act (FDASIA) in 2012, and later expanded by PAHPRA in 2013 for medical countermeasures. But it’s only used for drugs that are truly critical. Not every drug on the shortage list gets an extension. Only those where alternatives don’t exist or would harm patients.How the FDA Decides to Extend an Expiration Date
Manufacturers don’t just slap on a new date. They submit stability data to the FDA showing the drug still has the right strength, purity, and identity. The FDA reviews it. If the data holds up, they approve an extension. Most extensions add one year. But it’s not always that simple. In October 2024, the FDA allowed certain Baxter IV solutions to be used up to 24 months after manufacture-double the normal shelf life. That’s because the shortage was so severe, and the data showed those bags remained sterile and effective. The agency doesn’t require relabeling. That means a vial of Meperidine hydrochloride with an original expiration of September 30, 2025, can legally be used until January 30, 2026, even if the label doesn’t change. Pharmacies and hospitals have to check the FDA’s official list by lot number to know which ones are covered.Which Drugs Get Extended the Most
Some drugs are more likely to get extensions than others. Propofol tops the list-used in nearly every operating room. Epinephrine injections come next. These are drugs you can’t substitute easily. You can’t swap epinephrine for another adrenaline product without risking dosing errors or allergic reactions. Other common ones include:- Dantrolene sodium (for malignant hyperthermia)
- Ethiodized oil (for imaging procedures)
- Antivirals like Tamiflu and Relenza during flu outbreaks

What Hospitals and Pharmacies Must Do
This isn’t a free-for-all. Hospitals can’t just use any expired drug. They must:- Check the FDA’s public database daily
- Match the lot number on the vial or bag to the approved list
- Update pharmacy inventory systems to flag extended-date items
- Train staff to verify before administration
How This Fits Into Broader Shortage Solutions
Expiration date extensions are a band-aid, not a cure. The FDA also works with manufacturers to fix quality issues, speed up inspections, and find alternative suppliers. But when a factory shuts down or raw materials vanish, there’s no quick fix. The pandemic exposed how fragile the system is. Single-source production for generics made things worse. If one company makes 90% of a drug and their plant has a contamination issue? That’s a nationwide shortage. The FDA’s extended use program helps bridge the gap. It buys time. It keeps surgeries going. It keeps ICU patients alive. But it doesn’t fix why shortages happen in the first place.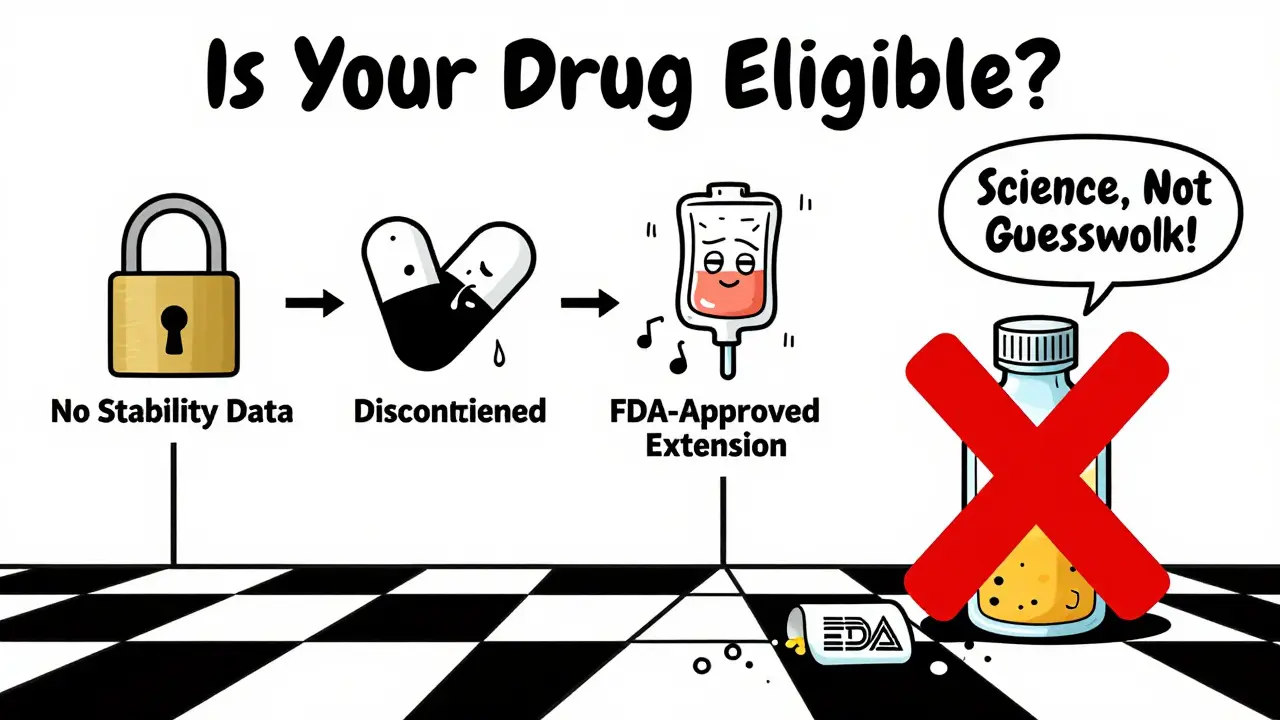
What’s Changing in 2026
The FDA still updates its drug shortage list daily. As of January 2026, IV fluid shortages remain a major issue, even as some other drugs stabilize. New manufacturers are stepping in for certain generics, but progress is slow. The agency has also started including medical devices on its shortage list-like empty IV bags-showing that the problem isn’t just about pills and injections. It’s about the whole supply chain. The bottom line? Extended expiration dates are a proven, regulated tool. They’re not risky guesswork. They’re science-based decisions made under pressure. And for patients who depend on these drugs, they’re often the only thing standing between life and a dangerous delay.How to Stay Updated
If you’re a clinician, pharmacist, or patient, the best place to check for active extensions is the FDA’s official Drug Shortages page. It’s updated daily and includes:- Current shortages
- Extended expiration dates by lot number
- Resolved shortages (kept for 6 months)
- Discontinued drugs (kept for 1 year)
What’s Not Allowed
The FDA doesn’t extend dates for:- Drugs without stability data
- Non-critical medications (like some antibiotics or pain relievers)
- Products with unknown manufacturing history
- Drugs that are already discontinued
Can any drug be used past its expiration date if there’s a shortage?
No. Only specific lots of specific drugs that the FDA has reviewed and approved for extension can be used past their printed date. The FDA publishes a detailed list with NDC numbers and lot numbers. Using any other expired drug is unsafe and illegal.
How long can a drug’s expiration date be extended?
Most extensions add one year, but some, like certain IV fluids, have been approved for up to 24 months past the original date. The length depends on the stability data submitted by the manufacturer and reviewed by the FDA.
Do hospitals have to relabel drugs with extended expiration dates?
No. The FDA does not require or recommend relabeling. Pharmacies must track extended-date lots using the FDA’s official list and update their inventory systems accordingly. Staff must verify lot numbers before use.
What happens when new supply arrives?
Once new, properly dated product becomes available, hospitals and pharmacies are expected to stop using the extended-date lots and dispose of them properly. The FDA considers these extensions temporary, not permanent.
Are extended expiration dates safe?
Yes, for the approved lots. The FDA only approves extensions when manufacturers provide rigorous stability data proving the drug maintains identity, strength, purity, and quality. These aren’t guesses-they’re science-backed decisions made under strict oversight.


Michael Burgess
January 3, 2026 AT 00:15Just saw a nurse in our ER use an extended-date epinephrine vial last week during a code. No one panicked. No one questioned it. The system worked. That’s the quiet heroism of this program - it doesn’t make headlines, but it saves lives when everything else is falling apart. 🙌
Palesa Makuru
January 4, 2026 AT 20:09Wow, so the FDA is basically playing god with expired meds now? I mean, I get it, but what’s next? Letting people drink expired milk because ‘the data says it’s fine’? 😏
Wren Hamley
January 5, 2026 AT 18:01That’s not how it works, Palesa. The FDA doesn’t just wing it - they require stability data from the manufacturer showing the drug still meets potency, purity, and sterility specs. Milk? No. IV fluids? Yes. The difference is science, not speculation.
And honestly, if you’ve ever had to watch a kid go into shock because the pharmacy was out of epinephrine, you’d appreciate this more than you’d like to admit.
Shruti Badhwar
January 7, 2026 AT 03:03The regulatory rigor here is astonishing. Manufacturers must submit accelerated and real-time stability data under ICH guidelines. The FDA’s review includes statistical analysis of degradation curves, microbiological integrity, and chemical assay validation. This isn’t bureaucracy - it’s pharmacokinetic due diligence.
And yet, the public perception remains dangerously simplistic. We treat this like a loophole, when in reality, it’s one of the most tightly controlled exceptions in modern medicine.
Let’s not forget: this program was born out of the 2011 heparin crisis, where contaminated batches led to deaths. The FDA didn’t create this to cut corners - they created it to prevent carnage.
When you’re running out of propofol and the only vial left is 3 months past its label date, but the stability data says it’s 99.8% intact - you don’t hesitate. You administer it. And you thank the scientists who made that possible.
This is the quiet infrastructure of survival. No fanfare. No press releases. Just a database update and a nurse double-checking a lot number before pushing the syringe.
It’s not about trust. It’s about evidence. And evidence, in this case, is the only thing standing between a patient and death.
The real scandal isn’t the extension - it’s that we need it at all. Single-source manufacturing is a structural flaw, not a coincidence. And until we fix that, we’ll keep relying on this elegant, fragile patch.
Lori Jackson
January 7, 2026 AT 03:21So let me get this straight - we’re letting hospitals use drugs past their expiration date… but only if the FDA says so? Who gave them that power? Who voted on this? This is socialist pharmaceutical control disguised as ‘science.’
And don’t even get me started on the fact that they don’t require relabeling. That’s how you get fatal errors. Someone’s going to die because a nurse didn’t check the damn database. And then we’ll all be crying about it.
This is a slippery slope. Next thing you know, we’ll be extending expiration dates for insulin because ‘it’s still good.’
Hank Pannell
January 7, 2026 AT 18:50There’s a profound epistemological tension here: we’re told to trust the data, not the label. But labels are the social contract of pharmaceutical safety. When the data overrides the label, what does that say about our faith in institutional authority?
And yet - if the data says it’s safe, and the alternative is death - then the label becomes a relic, not a rule.
This isn’t just about pharmacology. It’s about how we define risk in a world where certainty is a luxury we can’t afford.
Maybe the expiration date was never meant to be absolute. Maybe it was always a probabilistic estimate, and we just forgot that.
The FDA isn’t breaking the rules - they’re revealing their limitations.
Brittany Wallace
January 9, 2026 AT 14:37Wow. This is the kind of thing that makes me proud to be American. 🇺🇸 Not because it’s perfect - but because someone, somewhere, is quietly doing the math, checking the stability curves, and making sure a kid gets their IV fluids even when the world is falling apart. No fanfare. Just science. Just care.
Also - anyone else think we should have a national holiday for pharmacists? 🙏
Kerry Howarth
January 11, 2026 AT 08:26Exactly. This is how public health should work: evidence-based, transparent, and tightly controlled.
Angela Goree
January 12, 2026 AT 02:25STOP! This is dangerous! The FDA is overreaching! Who authorized them to override manufacturer dates?! This is tyranny disguised as public service! We need a congressional hearing - NOW!
Liam Tanner
January 13, 2026 AT 04:22I’ve worked in hospital pharmacy for 18 years. I’ve seen shortages where we had to ration IV fluids by the mL. I’ve watched residents cry because they couldn’t start an IV because the bags were all expired.
This program? It’s not glamorous. It’s not sexy. But it’s the reason your uncle survived sepsis last year. And the reason your kid got their surgery on time.
Don’t turn this into a political issue. Turn it into a lesson: fix the supply chain. Until then, let the scientists do their job.
Joy F
January 14, 2026 AT 15:37Oh, so now we’re trusting the FDA to be our pharmacists? How quaint. Meanwhile, the real crisis is that Big Pharma intentionally creates shortages to jack up prices. This ‘extension’ is just PR to make them look like heroes while they profit from the chaos.
Let’s not pretend this is about patient safety - it’s about corporate damage control wrapped in a lab coat.
Philip Leth
January 16, 2026 AT 02:18Man, I used to work in a rural ER. We had a batch of dantrolene that was 14 months past its date. We checked the FDA list. It was approved. We used it. Patient lived. No one ever knew. That’s the real story - not the drama, not the outrage. Just quiet, smart, safe medicine.
And yeah - we all had to learn how to use the database. No big deal. We’re professionals.
Sarah Little
January 16, 2026 AT 20:56Wait - so you’re saying we’re supposed to check the FDA’s database daily? For every single drug? That’s impossible. No hospital has the staffing for that. This policy looks good on paper, but it’s a logistical nightmare in practice.