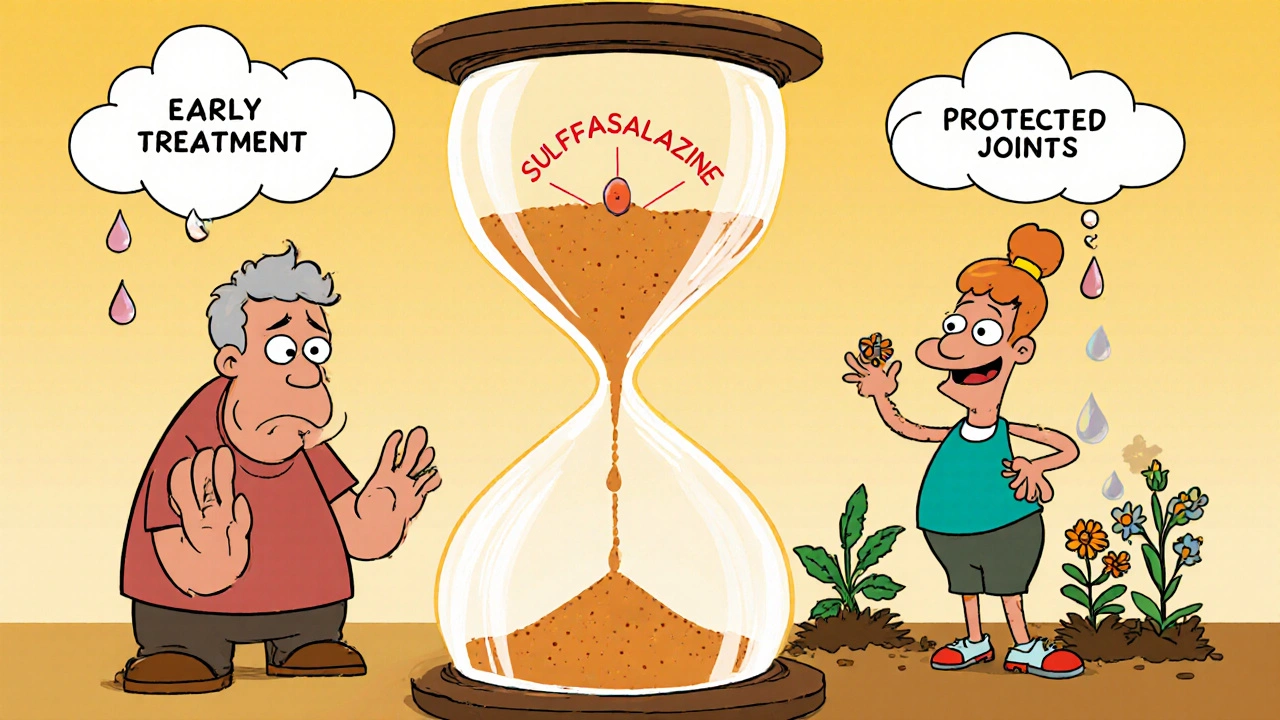
When you have rheumatoid arthritis, every morning can feel like a battle. Stiff joints, swelling, and that deep ache that won’t go away-it’s not just discomfort. It’s your body slowly tearing itself apart. And if nothing stops it, those joints can become permanently damaged, misshapen, and useless. That’s where sulfasalazine comes in. It doesn’t just ease pain. It actually slows or stops the damage before it becomes irreversible.
What Sulfasalazine Actually Does
Sulfasalazine is a disease-modifying antirheumatic drug, or DMARD. That means it doesn’t just mask symptoms like ibuprofen or naproxen. It targets the root cause: your immune system attacking your own joints. In rheumatoid arthritis, immune cells flood the synovium-the lining of your joints-and start chewing through cartilage and bone. Sulfasalazine breaks that cycle.
It works in two ways. First, it reduces inflammation by blocking certain chemicals in your body that signal immune cells to attack. Second, it slows down the overactive immune response that drives joint destruction. Studies from the Annals of the Rheumatic Diseases show that people taking sulfasalazine early in their disease had 40% less joint erosion on X-rays after two years compared to those on placebo.
It’s not a quick fix. You won’t feel better in a day. Most people start noticing less swelling and stiffness after 6 to 12 weeks. But that’s when the real work begins-preventing damage that can’t be undone.
Why Prevention Matters More Than Pain Relief
Painkillers are comforting, but they’re like putting a bandage on a leaking pipe. The water keeps flowing. Sulfasalazine is the plumber. It stops the leak.
Joint damage from rheumatoid arthritis isn’t just about looking different. It’s about losing function. Fingers can’t grip. Knees can’t bend. Wrists can’t turn. Once cartilage and bone are gone, no pill, no injection, no surgery can fully restore them. That’s why doctors push for early treatment with drugs like sulfasalazine.
A 2023 study tracking 1,200 patients over five years found that those who started sulfasalazine within six months of diagnosis were 65% less likely to need joint replacement surgery later on. That’s not a small number. That’s life-changing.
Who Benefits Most From Sulfasalazine
Sulfasalazine isn’t for everyone with arthritis. It’s most effective in people with moderate rheumatoid arthritis-those who have swelling in multiple joints, elevated inflammation markers like CRP or ESR, and no severe organ involvement.
It’s also commonly used in people with psoriatic arthritis, especially when skin and joint symptoms appear together. In those cases, it helps both the scaly patches on the skin and the painful, swollen joints.
But it’s not ideal for everyone. If you have a sulfa allergy, you can’t take it. That’s not rare-about 6% of the population reacts to sulfa drugs. Symptoms like rash, fever, or trouble breathing mean you need to stop immediately and switch to something else.
It’s also not the first choice if your disease is very aggressive. In those cases, doctors often start with methotrexate or biologics. But for many, sulfasalazine is the right balance: effective, affordable, and with a long safety record.
What to Expect When You Start Taking It
Starting sulfasalazine isn’t always smooth. The first few weeks can bring side effects: nausea, headache, dizziness, or upset stomach. These usually fade as your body adjusts. Taking it with food helps. So does starting with a low dose and slowly increasing it.
Your doctor will check your blood every few weeks at first. Sulfasalazine can lower white blood cell counts or affect liver function. That’s why monitoring matters. It’s not dangerous if caught early. Most people tolerate it well after the first month.
Some people notice their urine turns orange. It’s harmless-just a side effect of how the body breaks down the drug. Don’t panic. It’s not blood.
It’s also important to know: sulfasalazine doesn’t cure arthritis. But it can keep it quiet for years. Many people stay on it for decades with no major issues, as long as they’re monitored.
How It Compares to Other DMARDs
There are several DMARDs out there. Here’s how sulfasalazine stacks up:
| Drug | Time to Work | Common Side Effects | Cost (30-day supply, UK) | Joint Damage Reduction |
|---|---|---|---|---|
| Sulfasalazine | 6-12 weeks | Nausea, headache, orange urine | £15-£25 | High (40-60% reduction in erosion) |
| Methotrexate | 4-8 weeks | Liver stress, fatigue, mouth sores | £10-£20 | Very High (60-70% reduction) |
| Hydroxychloroquine | 3-6 months | Eye changes (rare), dizziness | £20-£30 | Moderate (20-30% reduction) |
| Leflunomide | 4-6 weeks | Diarrhea, hair loss, liver issues | £40-£60 | High (50-65% reduction) |
Sulfasalazine sits in the middle. It’s not the fastest, but it’s one of the safest and cheapest. For many, it’s the best place to start-especially if you’re young, have mild to moderate disease, and want to avoid stronger drugs for now.
What Happens If You Stop Too Soon
Some people stop taking sulfasalazine because they feel better after a few months. That’s a mistake.
Feeling better doesn’t mean the immune system has stopped attacking. The damage can still be happening under the surface. Stopping early increases your risk of flare-ups and permanent joint changes.
Studies show that people who stop sulfasalazine before 12 months have a 70% chance of relapse within six months. Those who stay on it for at least two years have a much better chance of long-term remission.
That’s why doctors recommend staying on it-even if you feel fine. Think of it like brushing your teeth. You don’t stop because your mouth doesn’t hurt anymore. You keep going because you’re preventing future problems.
When Sulfasalazine Isn’t Enough
Not everyone responds. About 30% of people don’t get enough benefit from sulfasalazine alone. That doesn’t mean it failed. It means it’s time to add something else.
Many patients combine it with low-dose methotrexate or hydroxychloroquine. This combo approach is common and often more effective than any single drug. In fact, the European League Against Rheumatism recommends combination DMARD therapy for patients who don’t reach treatment goals within 3-6 months.
If inflammation keeps creeping up, your doctor may add a biologic-like adalimumab or etanercept. These are powerful, but also expensive and require injections. Sulfasalazine often stays in the mix because it helps reduce the dose needed of the stronger drugs.
Real-Life Impact: What Patients Say
One woman from Glasgow, 52, started sulfasalazine after being diagnosed with rheumatoid arthritis at 48. She used to struggle to open jars. Her knuckles were swollen and red. After six months on the drug, her swelling dropped. After two years, her X-rays showed no new damage. She’s still working as a teacher. She didn’t get cured. But she kept her hands.
Another man from Edinburgh, 67, switched from ibuprofen to sulfasalazine after his doctor showed him his own X-rays-bone erosion in his wrists. He was skeptical. But after a year, his grip strength improved. He started gardening again. He says, "It didn’t make me young again. But it kept me from being broken."
These aren’t rare stories. They’re the reason sulfasalazine is still used in clinics today-decades after it was first approved.
Can sulfasalazine reverse existing joint damage?
No, sulfasalazine cannot repair bone or cartilage that’s already lost. Its job is to stop further damage. That’s why starting early is critical. Once erosion shows up on an X-ray, the focus shifts from reversal to prevention.
Is sulfasalazine safe for long-term use?
Yes, for most people. Long-term studies show it’s well-tolerated over 10+ years when monitored with regular blood tests. The biggest risks-low white blood cells or liver changes-are rare and usually caught early through routine checks.
Does sulfasalazine cause weight gain?
Not directly. Unlike steroids, sulfasalazine doesn’t trigger fluid retention or increased appetite. Some people gain weight because their inflammation drops and they feel better, so they eat more or move less. That’s not the drug’s fault-it’s a sign you’re improving.
Can I take sulfasalazine with other arthritis meds?
Yes. It’s often combined with methotrexate, hydroxychloroquine, or low-dose steroids. But avoid combining it with other sulfa drugs like some antibiotics or diuretics. Always tell your doctor about every medication you take.
How do I know if sulfasalazine is working?
You’ll notice less morning stiffness, fewer swollen joints, and more energy. But the real test is blood tests and imaging. Your doctor will track your CRP and ESR levels, and may order X-rays or ultrasound every 6-12 months to check for new bone erosion.
Next Steps: What to Do If You’re Considering Sulfasalazine
If you’ve been diagnosed with rheumatoid or psoriatic arthritis and haven’t started a DMARD yet, ask your rheumatologist about sulfasalazine. It’s not the flashiest drug, but it’s one of the most proven tools we have to protect your joints.
If you’re already on it and feeling better, don’t stop. Keep taking it. Keep your blood tests. Keep your appointments.
If you’re worried about side effects, talk to your pharmacist. They can help you manage nausea, suggest timing tips, or recommend alternatives if needed.
Joint damage from arthritis is silent. But it’s not inevitable. Sulfasalazine gives you control. Not over the disease-but over what it can take from you.


Jenn Clark
October 27, 2025 AT 20:45Sulfasalazine saved my hands. I could barely hold a coffee cup at 45. Now I knit again. It took months to work, but I didn’t give up. Worth every orange pee day.
Don’t stop just because you feel okay. The damage’s still whispering.
Trust the process.
L Walker
October 29, 2025 AT 10:05My GP tried to push me onto methotrexate straight away. Said sulfasalazine was 'old school'. I pushed back. Been on it 7 years. No liver drama. No injections. Just steady progress. Still working as a mechanic. Joints don't lie.
Don't let fancy new drugs scare you off the proven stuff.
giri pranata
October 29, 2025 AT 23:35Bro, I was skeptical too 😅 But after 3 months, my knuckles stopped looking like swollen grapes. Now I play guitar again! 🎸
Side effects? Yeah, nausea at first. Took it with food, went slow. No big deal.
And orange urine? LOL. I thought I was bleeding. Google saved me.
Do it. Your future self will high-five you.
PS: Don’t quit when you feel better. That’s when the real work starts!
Stuart Rolland
October 31, 2025 AT 17:43Let me tell you something about this drug-it’s not glamorous, it doesn’t come with a TikTok trend or a celebrity endorsement, but it’s one of the quiet heroes of rheumatology. I’ve seen patients come in with hands curled like claws, unable to button a shirt, and after a year on sulfasalazine, they’re planting gardens, holding grandkids, cooking meals without wincing. It doesn’t bring back what’s already gone, but it stops the erosion from turning into an avalanche. And that’s not just medicine-that’s dignity preserved. The cost? A fraction of a biologic. The impact? Life-altering. If you’re young, moderate disease, no sulfa allergy-start here. Let it do its slow, steady work. Don’t rush to the heavy artillery unless you have to. Sometimes the quietest tool is the one that lasts the longest.
And yes, the orange urine is weird, but it’s not blood. I promise.
Kent Anhari
November 2, 2025 AT 10:40My mom’s been on it for 15 years. Still works. Blood tests every 3 months. No drama. She says it’s like having a bodyguard inside her immune system. Funny, but true.
Charlos Thompson
November 2, 2025 AT 19:26Oh great, another ‘sulfasalazine is magic’ cult post. Let me guess-you also think fluoride is a government plot and that eating kale cures cancer? Cool. I’ll stick with my biologics, thanks. At least they work in under 6 weeks. This thing’s like waiting for a fax machine to load a webpage.
Peter Feldges
November 3, 2025 AT 09:10While I appreciate the clinical rigor of this post, I must respectfully note that the assertion regarding ‘40% less joint erosion’ is statistically significant but not necessarily clinically transformative in all populations. Furthermore, the cost comparison table omits regional variability in drug pricing-particularly in the U.S., where even £15 may equate to $50+ without insurance. Additionally, the ‘orange urine’ side effect, while benign, is frequently misinterpreted by patients as hematuria, leading to unnecessary ER visits. Perhaps a more nuanced discussion of patient education and adherence barriers is warranted before universal endorsement?
Rohit Nair
November 3, 2025 AT 10:21bro i started this med last year and my fingers dont hurt anymore when i type 😭
but man the first month was rough like i thought i was gonna die
took it with dinner and it got better
orange pee scared me at first but google said its fine
my doc said keep going even if i feel good
so i did
now i can lift my kid again
thank you sulfasalazine
Wendy Stanford
November 4, 2025 AT 22:24It’s fascinating how we’ve reduced human suffering to a pharmacological algorithm. We don’t ask why the immune system turns against itself-we just suppress it with chemicals. We don’t explore diet, stress, trauma, or environmental toxins-we just prescribe another pill. Sulfasalazine may slow erosion, but it doesn’t heal the wound in the soul that comes with chronic illness. You’re not just treating joints-you’re treating a person who’s been told their body is broken. And maybe, just maybe, the real damage isn’t in the cartilage-it’s in the belief that a pill can fix everything.
Jessica Glass
November 5, 2025 AT 01:56Oh wow, someone actually wrote a post that doesn’t say ‘just take ibuprofen and tough it out’? Revolutionary. Next you’ll tell me exercise helps. I’m sure the pharmaceutical reps are thrilled. Meanwhile, people with real RA are stuck choosing between bankruptcy and being crippled. Thanks for the ‘affordable’ drug-when your insurance denies it, it’s $300 a month. And no, I don’t care about your orange pee.
Krishna Kranthi
November 5, 2025 AT 10:44Man this drug is like that old bike you fix up-won’t win races but gets you from A to B without falling apart. Orange pee? Yeah, I thought I was dying too 😂 But after 8 months, my wrists stopped looking like sausages. Still got my job as a painter. Still paint. Still alive. Sulfasalazine ain’t sexy but it’s loyal. And hey-if your doc says ‘try it first’, they’re not being lazy. They’re being smart.
Lilly Dillon
November 5, 2025 AT 19:19I’ve been on it for 9 years. No flares. No new damage. Still walk my dog every morning. I didn’t know how much I missed that until I could do it again. I don’t talk about it much. It’s just… quiet relief.
Shiv Sivaguru
November 6, 2025 AT 11:58So you’re telling me this cheap pill stops joint damage? Then why is everyone on biologics? Sounds like a scam. Probably just a placebo with side effects. My cousin tried it and said it made him feel worse. You guys always overhype these things.
Gavin McMurdo
November 6, 2025 AT 17:50Let’s be real: sulfasalazine isn’t the answer-it’s the *compromise*. It’s what you take when you can’t afford the fancy stuff, when your insurance won’t cover biologics, when your doctor’s too busy to dig deeper. It’s the Band-Aid on a hemorrhage. And don’t get me started on the ‘orange urine’ as some harmless quirk-it’s a red flag you’re metabolizing a toxin. The fact that we’re still using this in 2024 is a indictment of our healthcare system, not a victory. You call it ‘affordable’? I call it ‘acceptable suffering’. And no, I won’t be taking it. I’d rather risk the biologic’s cost than accept a slow, silent erosion of my body as ‘normal’.