Every year, over 1.5 million people in the U.S. are harmed by mistakes in how their prescriptions are written. These aren’t rare accidents-they’re preventable errors that happen before the medicine even leaves the doctor’s office. And the worst part? You don’t have to wait for something to go wrong. As a patient, you can catch these mistakes before they hurt you.
What Are Prescription Writing Errors?
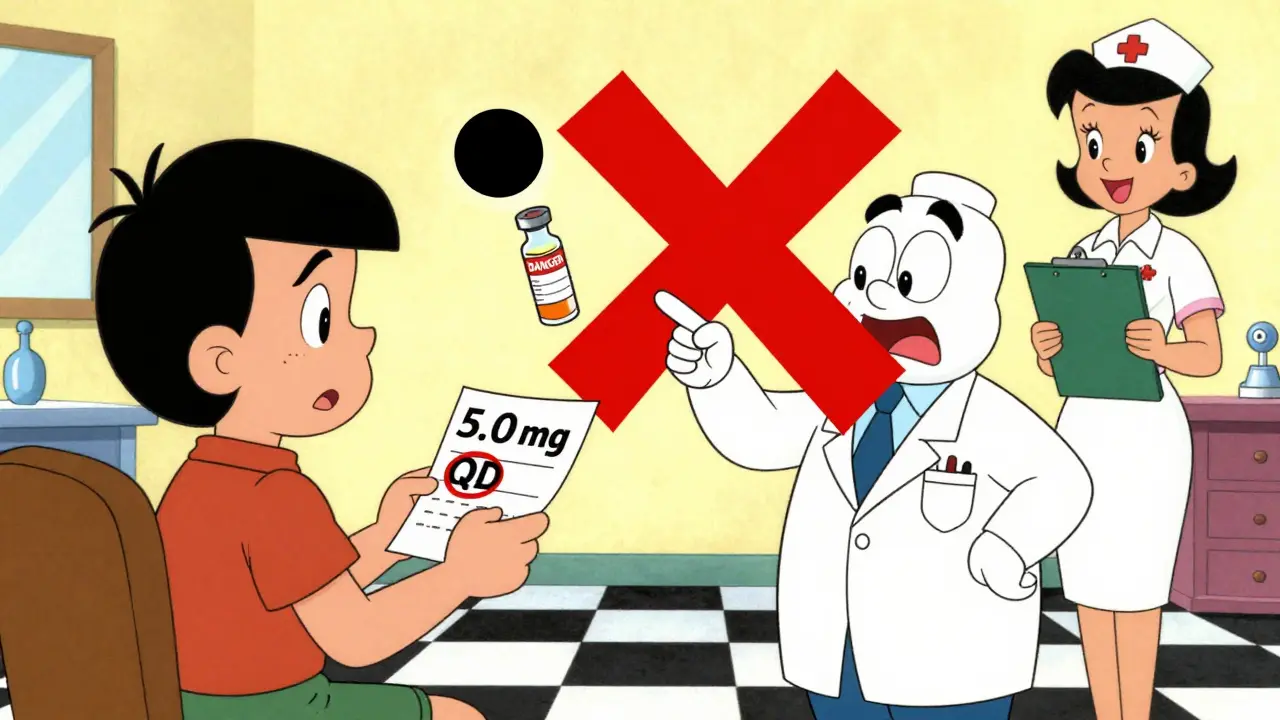
A prescription writing error is any mistake made when a doctor or provider writes out your medication order. It could be a wrong dose, a confusing abbreviation, or even the wrong drug entirely. These errors don’t always come from carelessness. Often, they’re caused by time pressure, tired providers, or outdated habits like using shorthand that sounds fine to them but is dangerous to you. According to data from the National Coordinating Council for Medication Error Reporting and Prevention, these errors happen during the prescribing phase-before the pharmacy even gets involved. That means you’re the first line of defense. The most common types of errors include:- Wrong dosage (19% of errors)-like writing 5.0 mg instead of 5 mg, which can be read as 50 mg.
- Illegible handwriting (22% of errors)-still a problem even in the digital age, especially in urgent care or rural clinics.
- Incorrect drug name (7% of errors)-mixing up drugs that sound or look alike, like Celebrex and Celexa, or Zyprexa and Zyrtec.
- Bad abbreviations-things like “U” for units (can be mistaken for “0”), “QD” for daily (confused with “QID” for four times a day), or “ug” for micrograms (read as “units,” leading to deadly insulin overdoses).
- Missing or unclear instructions-like not saying whether to take the pill with food, or how often.
High-Alert Medications Are the Most Dangerous
Not all medications carry the same risk. Some are called “high-alert” because even a small mistake can kill you. These include:- Insulin
- Anticoagulants (like warfarin or heparin)
- Opioids (like oxycodone or fentanyl)
- Chemotherapy drugs
- IV potassium chloride
Seven Things to Check on Every Prescription
The FDA recommends a simple checklist you can use every time you get a new prescription. Do this before you leave the office-or as soon as you get the paper or digital copy:- Full drug name-Is it written out completely? No abbreviations like “Lantus” when it should be “insulin glargine.”
- Precise dosage-Does it say “0.5 mg” and not “.5 mg”? Never trust a number without a leading zero. And never see “5.0 mg”-that trailing zero can be mistaken for 50 mg.
- Clear frequency-Does it say “take once daily” instead of “QD”? “BID” should be “twice daily.” Avoid abbreviations entirely.
- Total quantity-If you’re supposed to take a pill once a day for 30 days, does the prescription say 30 pills? If it says 100, that’s a red flag.
- Purpose of the medication-Is it written why you’re taking it? “For high blood pressure” or “for anxiety” helps you catch if the wrong drug was prescribed.
- Prescriber’s contact info-If the phone number is missing or looks wrong, call the office to confirm.
- Expiration date-Prescriptions expire. If it’s dated more than a year ago, don’t fill it.
Watch for These Dangerous Abbreviations
Some abbreviations are so dangerous they’ve been banned in hospitals. But they still show up in handwritten or poorly designed electronic systems. Here’s what to look for:- “U” for units → Always spell out “units.”
- “QD,” “QID,” “BID” → Use “daily,” “four times daily,” “twice daily.”
- “MS” or “MSO4” → Could mean morphine sulfate or magnesium sulfate. One calms pain, the other stops heartbeats. Never guess.
- “HC” → Could be hydrocortisone or heparin. One treats skin rashes, the other prevents blood clots.
- “Trailing zero” → “5.0 mg” → Always write “5 mg.”
- “Leading zero” missing → “.5 mg” → Always write “0.5 mg.”
Use the “Teach-Back” Method
When your doctor or nurse explains how to take your medicine, don’t just nod and say “yes.” Repeat it back in your own words. This is called the “teach-back” method-and it’s proven to cut misunderstandings by 81%. Try this:“So just to make sure I got it right-you want me to take one 5 mg tablet every morning with breakfast, right? And I shouldn’t crush it?”If they hesitate or correct you, you’ve just caught a mistake. If they say “yes,” you’ve got clarity. Either way, you’re safer.
Ask the “Ask Me 3” Questions
The National Patient Safety Foundation created a simple three-question framework that works every time:- What is my main problem? (What condition is this medicine for?)
- What do I need to do? (How and when do I take it?)
- Why is it important for me to do this? (What happens if I skip it or take too much?)
Check Your Electronic Prescriptions Too
Yes, e-prescribing cut handwriting errors by 55%. But it created new problems. A 2019 JAMA study found electronic systems caused 34% of new error types. Why? Dropdown menus. If your doctor is rushing and clicks “50 mg” instead of “5 mg” because it’s right below it on the list, you’re at risk. Or if the system auto-fills “Lisinopril” but you’re allergic to “Lisinopril HCTZ,” you might get the wrong combo. Always verify the electronic prescription matches what your doctor told you. When you get the label at the pharmacy, compare it to your notes. If the name, dose, or frequency doesn’t match-ask.
Use Technology to Your Advantage
There are now apps like MedSafety and MyTherapy that let you take a photo of your prescription. They use AI to scan for common errors-wrong doses, dangerous abbreviations, look-alike drug names. In a 2023 pilot study, these apps helped patients catch 68% more errors than those who didn’t use them. Also, under new 2025 rules, all electronic health records must give you real-time access to your prescriptions through secure apps. If your doctor uses a modern system, you should get an alert or message the moment your prescription is sent. Use it. Check it. Confirm it.What If You Spot an Error?
Don’t panic. Don’t ignore it. Don’t just assume the pharmacist will catch it. Call your doctor’s office. Say: “I got my prescription for [drug name], and the dose says [X mg], but I thought we agreed on [Y mg]. Can you confirm?” Pharmacists are trained to catch errors too. If they look confused or say “this doesn’t look right,” trust them. Ask them to call your doctor. Most pharmacies now spend nearly 20 minutes per prescription just verifying orders-because so many come in wrong.Why This Matters More Than You Think
Prescription errors are the #1 cause of preventable harm in healthcare. They cost the U.S. system $42 billion a year. They’re behind 21% of all medical malpractice claims. And yet, most patients never think to check. You’re not just a passive recipient of care. You’re a critical part of the safety system. Your eyes, your questions, your voice-these are tools as powerful as any algorithm or electronic alert. The future of medication safety isn’t just better software. It’s better patients. People who know what to look for. People who aren’t afraid to ask. People who understand that their life might depend on a single decimal point.What’s Next?
By 2030, experts predict 90% of prescriptions will require patient confirmation before they’re filled. That means you’ll be asked to log in, tap “I confirm,” or even record a short video saying you understand your meds. That’s not dystopian. That’s necessary. And you can start doing it today.Can I get a copy of my prescription before going to the pharmacy?
Yes. Under current federal rules, you have the right to receive a printed or digital copy of your prescription before leaving the doctor’s office. Ask for it. If they say no, ask why. Many clinics now send it via secure patient portals. Use this copy to check for errors before you go to the pharmacy.
What should I do if the pharmacy says my prescription is wrong?
Don’t argue. Don’t leave without answers. Ask the pharmacist to call your doctor’s office. Most pharmacies have direct lines to prescribers. If the doctor made a mistake, the pharmacist will fix it. If it’s a system error, they’ll correct it. Either way, you’ve prevented harm. Never feel bad for asking.
Are handwritten prescriptions still common?
They’re rare in hospitals and large clinics, but still used in some urgent care centers, rural practices, and by older providers. Even in digital systems, some doctors print and sign prescriptions manually. Always check for illegible writing, unclear numbers, or strange abbreviations. If you can’t read it, don’t fill it.
Can I use my phone to scan my prescription for errors?
Yes. Apps like MedSafety, MyTherapy, and even some pharmacy apps now let you take a photo of your prescription. They use AI to flag dangerous abbreviations, decimal errors, and look-alike drug names. In trials, these tools helped patients catch nearly 70% more errors than those who didn’t use them.
What if I don’t understand medical terms?
You don’t need to. Ask for plain language. Say: “Can you explain this in simple terms?” or “What does this drug do for me?” If your doctor can’t explain it simply, that’s a red flag. You have the right to understand your treatment. Don’t let jargon scare you into silence.