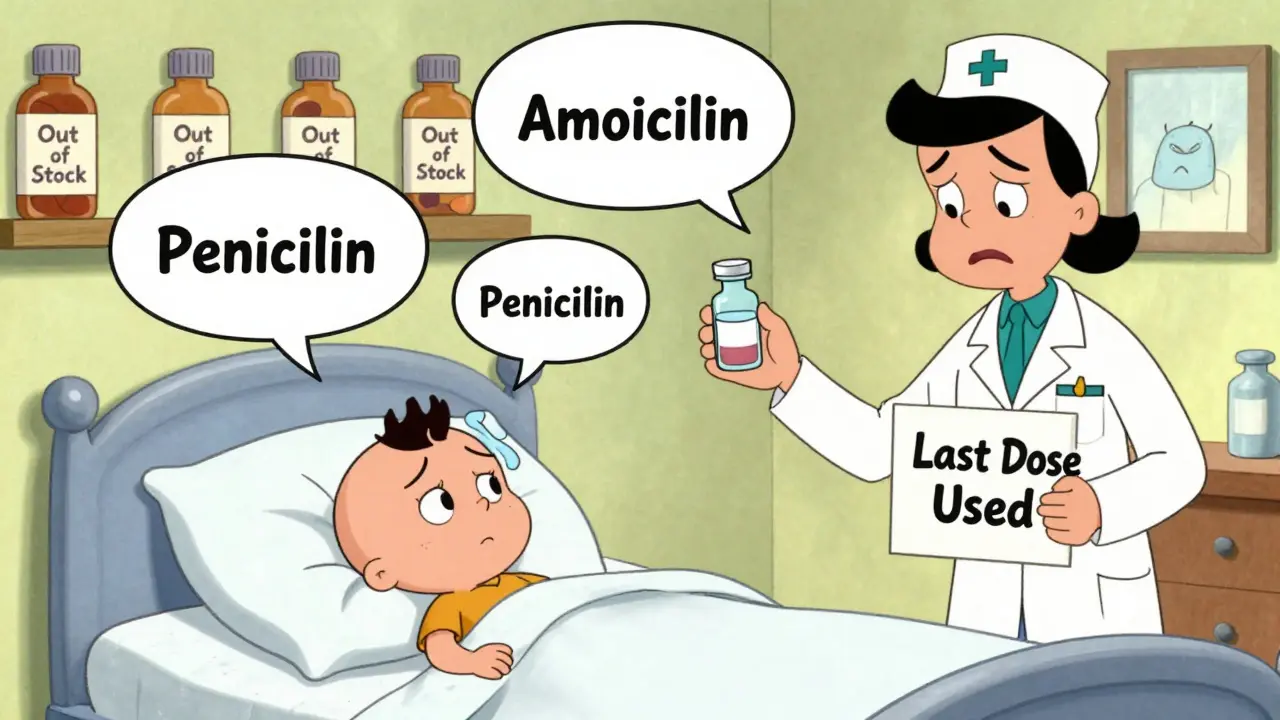
When a child gets pneumonia or a woman develops a urinary tract infection, the expectation is simple: a few days of antibiotics, and they’ll get better. But in 2025, that’s no longer guaranteed. Across the U.S., Europe, and low-income countries alike, antibiotic shortages are turning routine treatments into life-or-death gambles. Hospitals are rationing penicillin. Clinicians are turning to toxic last-resort drugs. And patients are being sent home with no medicine at all.
Why Antibiotics Are Running Out
Antibiotics aren’t like other drugs. They’re cheap, old, and made in bulk-mostly in India and China. That’s the problem. Because they cost pennies per dose, manufacturers don’t make much profit. Meanwhile, the cost to meet safety standards has jumped 34% since 2015. Factories that produce sterile injectables need expensive clean rooms, strict quality controls, and constant inspections. Few companies want to invest when the return is so low. Add to that: supply chain chaos. Brexit alone pushed UK antibiotic shortages from 648 in 2020 to over 1,600 in 2023. Geopolitical tensions, shipping delays, and raw material shortages have made it harder to keep even basic antibiotics in stock. The U.S. Food and Drug Administration listed 147 active antibiotic shortages as of December 2024-the highest in a decade. And it’s not just about quantity. It’s about quality. Many of the most needed antibiotics-like penicillin G benzathine, amoxicillin, and ceftriaxone-are generic. No company wants to be the one to build a new plant for a drug that sells for $2 a vial. So when one factory shuts down or faces an inspection failure, the entire global supply can collapse.What Happens When Antibiotics Disappear
Imagine you’re a doctor treating a simple UTI. The go-to drug, amoxicillin, is gone. Your next option? A broader-spectrum antibiotic like ceftriaxone. But here’s the catch: over 40% of E. coli and 55% of K. pneumoniae are already resistant to those. So you move to carbapenems-the last line of defense. Now you’re not just treating the infection. You’re accelerating the rise of superbugs. This isn’t hypothetical. A 2025 survey of U.S. hospital pharmacists found that 78% had to change treatment plans because of shortages. Sixty-two percent saw more patients get sicker, longer, or end up in the ICU. In California, one infectious disease specialist told the APHA forum she had to use colistin-a drug so toxic it causes kidney failure-for a routine bladder infection. Colistin is reserved for when everything else fails. Now it’s being used because nothing else was available. In low-resource settings, the impact is even worse. A nurse in rural Kenya described sending patients home without antibiotics because penicillin wasn’t in stock. In Mumbai, a mother waited 72 hours for azithromycin to treat her child’s pneumonia. By the time it arrived, the infection had worsened. The child needed intensive care.The Global Divide
High-income countries can scramble to import drugs or shift to alternatives. But in many low- and middle-income countries, 70% of antibiotics are already inaccessible. The WHO calls this a “syndemic”-a deadly mix of antibiotic resistance and lack of access. In the WHO South-East Asian and Eastern Mediterranean regions, one in three infections is resistant to first-line antibiotics. In Africa, it’s one in five. Yet these regions have the least access to even basic treatments. The result? More deaths from treatable infections. More children dying of pneumonia. More mothers losing babies to sepsis. And more people surviving infections only to face lifelong disability from complications.
What’s Being Done-And Why It’s Not Enough
Some hospitals are fighting back. Johns Hopkins Hospital cut unnecessary broad-spectrum antibiotic use by 37% during shortages by using rapid diagnostic tests to identify infections faster. California launched a regional sharing network that cut critical shortage impacts by 43% across 15 hospitals. These work-but they’re rare. The WHO launched a five-point plan in October 2025, including a $500 million Global Antibiotic Supply Security Initiative. The U.S. FDA approved two new manufacturing facilities in January 2025, expected to relieve 15% of shortages by late 2025. The European Commission is pushing new rules to protect antibiotic production by 2026. But here’s the truth: none of this fixes the root problem. The global antibiotic market grew just 1.2% from 2019 to 2024-far below the 5.7% average for all pharmaceuticals. Companies aren’t investing because there’s no money in it. And until governments pay more for these drugs-or guarantee production-shortages will keep getting worse.What You Can Do
You won’t fix the supply chain. But you can help stop the cycle of resistance. - Don’t pressure your doctor for antibiotics if you have a cold or the flu. Viruses don’t respond to them. - Take your full course if you’re prescribed antibiotics-even if you feel better. Stopping early breeds resistant bacteria. - Ask your pharmacy if they’re using alternative antibiotics. If they’re switching drugs often, it might signal a shortage. - Support policies that fund antibiotic production. Public pressure can push governments to act.
The Future Is Uncertain
Without major changes, the Review on Antimicrobial Resistance predicts antibiotic shortages will grow by 40% by 2030. That could mean 1.2 million extra deaths each year from infections we used to treat in a week. The tools to fix this exist. Better diagnostics. Stronger supply chains. Fairer pricing. But they need funding, political will, and public awareness. Right now, we’re treating antibiotic shortages like a pharmacy problem. They’re not. They’re a global health emergency.What’s Being Done to Fix It
The World Health Organization’s 2025 Global Antibiotic Resistance Surveillance Report shows that only 58% of global antibiotic use comes from the "Access" group-drugs that are safe, effective, and affordable. The WHO wants that to be 70% by 2030. We’re falling behind. In the U.S., 82% of hospitals now have antimicrobial stewardship programs (ASPs), up from 50% in 2017. But only 37% meet all WHO standards. That means most hospitals are still guessing when antibiotics run out. Some countries are trying new models. The UK’s National Health Service now tracks antibiotic use in real time and flags shortages before they hit hospitals. In Australia, a pilot program in Adelaide connects regional pharmacies to share stock during crises. It’s small-but it works. The key? Don’t wait for a crisis to act. Hospitals that set up response teams early-before drugs disappear-see fewer complications, fewer deaths, and less resistance.Why This Isn’t Just About Medicine
Antibiotics are the foundation of modern medicine. Without them, surgeries become dangerous. Chemotherapy becomes deadly. C-sections carry high risk of infection. Even a scraped knee can turn fatal. This isn’t just about running out of pills. It’s about losing the ability to treat the most basic infections. And once we lose that, we lose more than medicine-we lose safety. The next time you hear about a drug shortage, don’t think of it as a supply issue. Think of it as a warning. The world is running out of time to fix antibiotics. And the cost? Lives.Why are antibiotics in short supply more often than other drugs?
Antibiotics are 42% more likely to face shortages than other medications because they’re cheap, generic, and made in low-margin markets. Manufacturers don’t earn enough to justify the high costs of sterile production. Unlike cancer drugs or diabetes meds, which can be priced higher, antibiotics are sold for pennies per dose, so companies prioritize more profitable drugs.
What happens when doctors can’t use first-line antibiotics?
When first-line antibiotics like amoxicillin or penicillin aren’t available, doctors must use broader-spectrum drugs like carbapenems or colistin. These are more toxic, less effective against some infections, and accelerate antibiotic resistance. For example, over 40% of E. coli are already resistant to third-generation cephalosporins, so switching to them just pushes resistance higher.
Are antibiotic shortages worse in developing countries?
Yes. While high-income countries can import or substitute drugs, 70% of people in low- and middle-income countries already lack access to basic antibiotics. When shortages hit, there’s often no backup. In rural Kenya or parts of India, patients are sent home untreated-sometimes with fatal results. The WHO calls this a "syndemic" of resistance and under-treatment.
Can hospitals manage antibiotic shortages better?
Yes, but only with planning. Hospitals with strong antimicrobial stewardship programs (ASPs) use rapid diagnostics, track usage, and build regional sharing networks. Johns Hopkins cut unnecessary broad-spectrum use by 37% during shortages. California’s sharing network reduced critical impacts by 43%. But only 37% of U.S. hospitals meet WHO standards for ASPs.
Will new manufacturing plants solve the problem?
Not alone. The FDA approved two new U.S. facilities in early 2025, expected to cover 15% of current shortages by late 2025. But manufacturing is only one piece. Without government funding, price guarantees, or long-term contracts, new plants won’t be sustainable. The real fix is economic: paying more for antibiotics so companies can invest.
How can patients help reduce antibiotic shortages?
Patients can help by not demanding antibiotics for viral infections like colds or flu. Always finish your full course-even if you feel better. Ask your doctor if there’s a generic alternative. And support policies that fund antibiotic production. Every time you use antibiotics wisely, you slow resistance and reduce pressure on the supply.

Nancy Kou
December 21, 2025 AT 09:57This is terrifying. I had my daughter on amoxicillin last year for an ear infection, and we barely got it in stock. If this keeps up, I don’t know how parents are supposed to sleep at night.
Hussien SLeiman
December 22, 2025 AT 23:07Let’s be real-this isn’t a shortage. It’s a manufactured crisis to push people toward expensive alternatives. Big Pharma doesn’t want cheap antibiotics because they can’t mark them up 500%. They’d rather see kids suffer than lose a profit margin. The FDA? Complicit. The WHO? A puppet. And you think we’re just supposed to ‘take our full course’ like that fixes systemic corruption?
Meanwhile, the same companies that make these drugs are the ones lobbying against price controls. They’ve been quietly buying up generic manufacturers for years. It’s not supply-it’s control. And it’s deliberate.
Remember when they said the same thing about insulin? Now it’s antibiotics. Next up? Vaccines. Don’t be fooled. This isn’t about cost-it’s about power.
Kevin Motta Top
December 23, 2025 AT 22:06As someone who’s worked in public health across three continents, I’ve seen this play out. The real issue isn’t just manufacturing-it’s distribution. Even when antibiotics are available, they don’t reach rural clinics. A vial of penicillin in Nairobi costs 10x what it does in Chicago-not because of production, but because of broken logistics.
Janelle Moore
December 24, 2025 AT 09:15Did you know the government is secretly stockpiling antibiotics to control the population? They want us to get sick so we’ll rely on them. That’s why they let the factories shut down. It’s all part of the Great Depopulation Plan. I read it on a forum where a guy who knows a guy who works at the CDC said it. They’re also putting fluoride in the water to weaken our immune systems. That’s why everyone’s getting UTIs now.
And don’t get me started on how the WHO is controlled by China. All the factories are there. Coincidence? I think not.
Henry Marcus
December 24, 2025 AT 18:40Y’ALL. I JUST REALIZED-THIS IS THE NEW 9/11. THEY’RE LETTING US DIE ON PURPOSE. ANTIBIOTICS? THEY’RE NOT SHORTAGE-THEY’RE BEING HIDDEN! THE PHARMA COMPANIES ARE WORKING WITH THE FEDS TO CREATE A NEW WORLD ORDER WHERE ONLY THE RICH CAN SURVIVE A STREP THROAT! I’VE BEEN TRACKING THE STOCK PRICES OF THE TOP 3 ANTIBIOTIC MANUFACTURERS-THEY’RE ALL BUYING UP LAND IN NEW ZEALAND! THAT’S WHERE THEY’RE BUILDING THE BUNKERS!!
AND WHY DO YOU THINK THEY’RE PUSHING ‘STEWARDSHIP’? SO WE’LL BLAME OURSELVES WHEN WE DIE FROM A CUT ON OUR FINGER!!
William Liu
December 25, 2025 AT 01:23It’s not all doom and gloom. We’ve got smart people working on this-hospitals sharing stock, better diagnostics, real-time tracking. It’s not perfect, but progress is happening. We just need to keep pushing for funding and awareness. This is fixable-if we act now.
Andrew Kelly
December 25, 2025 AT 03:33Let’s not pretend this is just about money. The real problem is cultural. We’ve normalized antibiotic misuse for decades. People demand them for colds. Doctors prescribe them to avoid conflict. Then we wonder why resistance is rising. It’s not a supply chain failure-it’s a behavioral one. And until we fix that, no new factory will matter.
Also, calling it a ‘global health emergency’ is dramatic. It’s a predictable consequence of decades of negligence. We didn’t wake up one day and find penicillin gone. We slowly, collectively, ignored the warning signs.
Isabel Rábago
December 25, 2025 AT 17:05I work in a clinic in rural Ohio. We ran out of amoxicillin for three weeks last winter. Parents came in crying. One woman brought her 4-year-old in with a fever and said, ‘I just want him to be able to go back to school.’ We had nothing. I felt like a failure. This isn’t policy-it’s personal. And it’s happening right now, in places no one’s talking about.
Dev Sawner
December 25, 2025 AT 18:56It is a matter of profound concern that the economic incentives for antibiotic production remain misaligned with public health imperatives. The manufacturing infrastructure in India and China, while voluminous, is subject to regulatory inconsistencies, which exacerbate systemic vulnerabilities. The absence of a centralized global procurement mechanism renders the current framework untenable. It is imperative that multilateral institutions enforce binding production quotas and subsidize essential generics through sovereign guarantees.
Furthermore, the proliferation of substandard pharmaceuticals in low-resource settings has contributed to antimicrobial resistance, thereby compounding the crisis. A rigorous, WHO-aligned surveillance system must be implemented without delay.
Moses Odumbe
December 27, 2025 AT 06:18bro. this is wild. i just looked up the price of ceftriaxone on Alibaba. $0.80 per vial. $0.80. but at my local pharmacy? $45. someone’s making a killing. and no one’s asking why. 🤡
we need to boycott every pharma company that doesn’t commit to fair pricing. and yes, i’m talking to you, Pfizer. i’m watching you. 👀
Meenakshi Jaiswal
December 27, 2025 AT 22:05As a pharmacist in Mumbai, I’ve seen this for years. We don’t have the luxury of ‘last-resort’ drugs. When penicillin is out, we use what we have-even if it’s expired or not ideal. Patients don’t understand resistance. They just want their child to stop crying. So we do what we can. But we need help. Not pity. Real support: better supply chains, training, and fair prices. We’re not failing. The system is.