Medication Adherence Suitability Checker
Assess Your Digital Pill Suitability
Based on your condition, medication type, and tech comfort, we'll help determine if digital pill sensors could be beneficial for you.
For millions of people taking daily medications for chronic conditions, forgetting a dose isn’t just a mistake-it’s a risk. Studies show that about half of patients don’t take their pills as prescribed. That’s not laziness. It’s forgetfulness, confusion, fear of side effects, or simply the weight of managing multiple drugs over years. Now, a quiet revolution is happening inside the stomach: digital pill sensors are turning swallowed tablets into data points, giving doctors real-time insight into whether a pill was taken-and even how the body responded.
How Digital Pills Actually Work
A digital pill isn’t magic. It’s a tiny sensor, smaller than a grain of rice, embedded inside a standard medication capsule. When you swallow it, stomach acid activates the sensor. Inside, copper and magnesium electrodes react, generating a small electric charge-just enough to send a unique signal. That signal gets picked up by a skin patch worn on your abdomen, which then sends the data to your phone via Bluetooth. The patch doesn’t just listen for the pill. It also tracks your heart rate and movement. Some advanced versions, like Philips’ IntelliCap, even measure stomach temperature and pH levels. All this data flows into a secure app or web portal, where your doctor or care team can see exactly when you took your medicine. No guesses. No self-reports. Just facts. The technology isn’t new. The FDA approved the first digital pill-Abilify MyCite, containing the antipsychotic aripiprazole-in 2017. Since then, systems from etectRx, Proteus Digital Health (now part of Medtronic), and others have been tested in trials for HIV, tuberculosis, heart disease, and diabetes. Each system uses similar core tech: a silicon-based sensor, BLE radio (Texas Instruments CC2541 chip), AES encryption for security, and a wearable patch with a 72-hour battery life.Why Adherence Data Matters More Than You Think
Medication non-adherence costs the U.S. healthcare system between $100 billion and $290 billion every year. That’s not just wasted pills-it’s avoidable hospital visits, worsening conditions, and premature deaths. Digital pills cut through the noise. In a 12-week trial with 157 patients on antipsychotic meds, adherence jumped from 62% to 84% when digital sensors were used. That’s not a small win. That’s life-changing. One patient with schizophrenia told a researcher: “Seeing the log made me realize I was skipping doses on weekends.” Another said, “It felt like my psychiatrist was watching me swallow pills.” Both reactions are real. The data isn’t just useful-it’s personal. And that’s where the tension lies. For patients with serious mental illness, epilepsy, or post-transplant regimens, missing a dose can mean a seizure, organ rejection, or relapse. In those cases, digital pills aren’t surveillance-they’re safety nets. But for someone managing high blood pressure or cholesterol, the same level of monitoring can feel invasive. A 2022 study found 73% of hesitant patients cited privacy as their top concern. And 61% said they felt “monitored,” not supported.Can Digital Pills Detect Side Effects?
This is where the tech gets really interesting. Early systems only confirmed ingestion. But the latest versions are doing more. The wearable patch tracks heart rate changes, activity drops, and sleep patterns. If your pulse spikes after taking a pill, or you suddenly stop walking for hours, the system flags it. In trials, these patterns have helped identify early signs of dizziness from blood pressure meds, fatigue from chemotherapy, or gastrointestinal distress from NSAIDs. The FDA approved a digital pill for tuberculosis treatment in March 2023-the first outside mental health. Why? Because TB treatment requires 6+ months of daily pills. Missing even a few doses can lead to drug-resistant strains. The digital system didn’t just track adherence-it helped catch side effects like nausea and liver stress before they became emergencies. Researchers are now building AI models that predict side effects before patients even notice them. etectRx partnered with IBM Watson Health in late 2023 to train algorithms that analyze historical data, daily movement, and vital signs to predict adherence lapses with 82% accuracy. The same models are being adapted to predict nausea, dizziness, or arrhythmias triggered by specific drugs.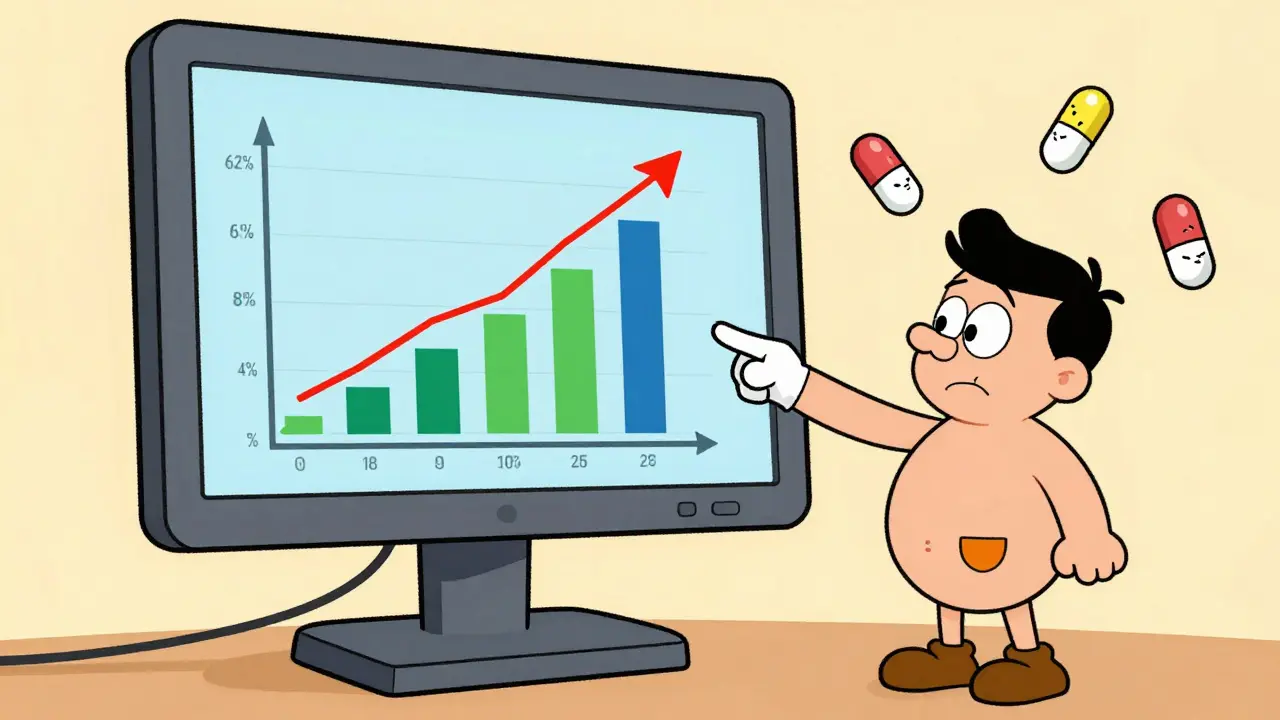
Who’s Using This-and Who Isn’t
Right now, digital pills are mostly used in clinical trials (78% of deployments) and specialized mental health clinics. Otsuka’s Abilify MyCite holds 52% of the clinical mental health market. etectRx’s ID-Cap system leads in research settings with 38% share. But outside those niches? Adoption is slow. Why? Cost. A single digital pill can cost $50-$100 more than the regular version. Insurance rarely covers it. Medicare and most private plans don’t reimburse for the sensor component. That’s why only 12% of uses are direct-to-consumer. Most patients never hear about it unless their doctor brings it up. Elderly patients face another barrier: the smartphone app. In geriatric trials, 38% needed help pairing the patch or logging in. If you’re 72 and not tech-savvy, a digital pill that requires a phone isn’t a solution-it’s another hurdle.The Privacy Problem
The Electronic Frontier Foundation warned in 2020 that digital pill data could be exploited by insurers or employers. What if your insurer sees you skipped your antidepressant for three days? Could they raise your rates? What if your employer gets access to your sleep and activity patterns from the patch? HIPAA protects data sent through healthcare channels. But state laws vary. Fourteen U.S. states have added extra digital health privacy rules. And the patch data isn’t just about pills-it’s your heart rate, steps, even when you sleep. That’s a lot of personal info. Most apps don’t let you delete data. They archive it. Forever. Patients want transparency. They want to know who sees their data, how long it’s stored, and whether it can be shared without consent. Right now, that’s not always clear.
What’s Next?
By 2026, the Digital Medicine Society predicts 60% of digital pill systems will include side effect detection. That means pills won’t just tell your doctor you took them-they’ll tell you if they’re making you feel worse. New sensors are being tested to detect biomarkers in stomach fluid-like glucose spikes after diabetes meds or inflammation markers after anti-rheumatic drugs. Imagine a pill that tells you your liver is stressed before your blood test shows it. The market is growing fast-projected to hit $2.4 billion by 2029. But growth depends on solving three things: cost, usability, and trust. If digital pills become affordable, simple for older adults, and come with ironclad privacy controls, they could become standard for high-risk meds. For routine drugs? Probably not.Is This Right for You?
Ask yourself: Do I have a condition where missing a dose could be dangerous? Am I comfortable with a device tracking my body data? Do I have someone who can help me with the app if I need it? If you’re on antipsychotics, immunosuppressants, TB meds, or complex cancer regimens, this tech might be a game-changer. If you’re on a daily statin or blood pressure pill? Maybe not yet. Talk to your doctor. Ask: “Is there a digital version of my medication? What data does it collect? Who sees it? Can I turn it off?” This isn’t about being watched. It’s about being understood. The goal isn’t to catch you skipping pills. It’s to help you take them without guilt, fear, or guesswork.How do digital pill sensors actually know I swallowed my medicine?
The sensor inside the pill activates when it hits stomach acid. It generates a tiny electric signal using a reaction between magnesium and copper electrodes. That signal is picked up by a wearable patch on your skin, which then sends the data to your phone. It confirms ingestion-not absorption. So it tells you the pill was swallowed, not whether your body absorbed it.
Can digital pills detect side effects like dizziness or nausea?
Not directly. But they can detect changes in your body that often accompany side effects. For example, if your heart rate spikes or your daily steps drop sharply after taking a pill, the system flags it. AI models are being trained to link these patterns to known side effects like dizziness or fatigue. In trials, this has helped catch reactions before patients even realize something’s wrong.
Are digital pills covered by insurance?
Almost never. Most insurance plans, including Medicare, cover the medication but not the sensor or patch. The added cost can be $50-$100 per pill. That’s why digital pills are mostly used in clinical trials or specialized care settings-not routine prescriptions.
Is my data safe with digital pill systems?
Data is encrypted during transmission using AES standards and stored on secure servers. HIPAA applies if the system is used through a healthcare provider. But state laws vary-14 states have stricter digital health privacy rules. You should always ask who owns the data, how long it’s kept, and whether it can be shared with insurers or employers.
Can I stop using a digital pill if I change my mind?
Yes. You can stop wearing the patch at any time. The sensor inside the pill passes through your system naturally and doesn’t stay in your body. But once data is sent to the server, it may still be stored unless you request deletion. Always check the provider’s privacy policy before starting.
Do digital pills work for elderly patients?
They can, but they’re harder to use. In trials, 38% of patients over 65 needed help connecting the patch to their phone or using the app. Simpler interfaces, voice-guided setup, and caregiver access features are being developed. For now, digital pills work best when paired with a family member or caregiver who can assist with tech.
What happens if the patch falls off or loses signal?
Signal loss happens in 8-15% of cases, especially in patients with higher BMI or if the patch isn’t positioned correctly. The system will flag missed transmissions, but it won’t assume you skipped your pill. Your doctor will see the gap and may follow up. Some newer patches have better adhesion and signal boosters to reduce this issue.
Are there alternatives to digital pills for tracking adherence?
Yes. Smart pill bottles that record when opened, blister packs with timers, and simple smartphone reminder apps are cheaper and less invasive. But none offer the same level of proof that the pill was swallowed. Digital pills are the only method that confirms ingestion-not just access.


Emma Duquemin
December 28, 2025 AT 17:23This is wild. I never thought my pill could be a tiny spy in my stomach. But honestly? If it means I don’t end up in the ER again because I forgot my blood thinner on a Tuesday night, I’m all in. My grandma’s on warfarin and she’s got a whole system of alarms, sticky notes, and a cat that knocks over her pill organizer. A sensor that actually knows if she swallowed it? Game changer. I’d pay extra for that peace of mind.
Also, the part about detecting side effects? Like, if my heart goes nuts after a new med? That’s not just data-that’s a lifesaver. My cousin’s on chemo and she didn’t realize how bad the dizziness was until she passed out in the shower. If this tech could’ve flagged that before it happened… I’d cry happy tears.
Yeah, privacy’s a nightmare. But I’d rather my doctor know I’m struggling than have me ghost my meds until I’m back in ICU. We just need better transparency. Not surveillance. Support.
Also-can we talk about how cool it is that a copper-magnesium reaction in stomach acid makes a Bluetooth signal? That’s like sci-fi in my gut. I’m low-key obsessed.
Also also-why is this still $100 extra per pill? That’s insane. If it saves $50k in ER visits, why aren’t insurers screaming to cover it? Somebody’s getting rich off our suffering.
Also also also-can we make the app less terrifying for elderly folks? My uncle’s 78 and thinks ‘Bluetooth’ is a type of fish. He needs voice-guided setup. Not a PhD in tech.
Anyway. I’m not scared of the tech. I’m scared of the cost and the silence around it. Let’s fix that.
Kevin Lopez
December 29, 2025 AT 10:15Adherence metrics are a proxy for behavioral compliance, not therapeutic efficacy. The sensor confirms ingestion, not bioavailability. You’re optimizing for compliance, not clinical outcomes. The data is noisy, confounded by gastric motility, pH variability, and patch misalignment. 84% adherence in trials? That’s selection bias. Real-world adherence is still <20% for chronic regimens. This is a solution looking for a problem.
Duncan Careless
December 30, 2025 AT 17:44Interesting read. Honestly, I’d be nervous about this if I were on meds. Not because I’m hiding anything-but because my phone’s already a mess of notifications. Another thing to track? Feels like one more weight. I get the benefit for serious conditions, but for blood pressure? Nah. I’d rather just set a reminder. And the privacy stuff… yeah, that’s a real concern. My mate’s insurer raised his premium after he missed a few antidepressant doses. Not cool. I’d want to know exactly who’s seeing my data, and if I can delete it. No one should be archiving my stomach activity forever.
Also, patches falling off? I’d be so stressed about that. Would they think I’m skipping? Ugh. Too much pressure.
Samar Khan
January 1, 2026 AT 09:41OMG I’m SO done with this 🤮. So now my body’s being monitored like a lab rat? Like, I swallow a pill and suddenly my heart rate, sleep, steps, and stomach acid are all being logged?? 😭 I’m not a data point. I’m a human. And if my doctor sees I skipped my pill on a Friday night because I was drunk and sad? Are they gonna judge me?? 🙈 I just want to feel better, not be tracked like a criminal. This feels like digital gaslighting. And who’s storing this?? WHO?? 😤 I’m out. No thank you. #DigitalPillNightmare
Russell Thomas
January 3, 2026 AT 00:16Oh wow. So now if I don’t take my statin, my doctor gets a text? What’s next? A drone that drops your pill into your mouth? You people are obsessed with control. You think if you just track enough data, people will magically behave. Newsflash: humans aren’t robots. You can’t algorithm your way out of depression, fatigue, or existential dread. I take my meds when I feel like it. And if my doctor doesn’t like it? Tough. I’m not paying for a surveillance system to make me feel guilty about being human.
Also, ‘side effect detection’? So if I nap after my blood pressure med, the app thinks I’m ‘experiencing dizziness’? I’m tired. Not sick. Chill out.
And the cost? $100 extra? You’re literally charging people to be monitored like prisoners. This isn’t healthcare. It’s corporate control dressed in lab coats.
Jasmine Yule
January 4, 2026 AT 05:00I’m not gonna lie-I cried reading this. My mom’s on immunosuppressants after her transplant. She used to hide skipped doses because she was scared of disappointing her doctor. Then they tried the digital pill. She told me, ‘It didn’t make me feel watched. It made me feel seen.’ That’s the difference. This isn’t about punishment. It’s about connection.
And yeah, the tech’s not perfect. The patch fell off twice. The app crashed. But her care team called her when they saw the gap. They didn’t scold her. They asked, ‘What’s going on?’ And that’s what changed everything.
Privacy? Yes, we need better laws. But don’t throw the baby out with the bathwater. This tech is saving lives. We just need to make it kinder. Simpler. More human.
Also, if you’re scared of it? Talk to your doctor. Ask questions. Demand transparency. You don’t have to use it. But don’t dismiss it because it’s new. Some of us are living because of it.
And for the love of god, can we please get voice-guided apps for seniors? My mom needed me to set it up for her. That’s not a failure. That’s a design flaw.
Greg Quinn
January 4, 2026 AT 23:29It’s fascinating how we’ve turned medicine into a feedback loop. We used to trust the body. Then we trusted the doctor. Now we trust the algorithm. The pill doesn’t just deliver a drug-it delivers a narrative. ‘I took it.’ ‘I didn’t.’ ‘I felt something.’ The data becomes a story we tell ourselves about our own discipline, our own failure, our own survival.
But here’s the quiet truth: no sensor can measure the weight of loneliness that makes you skip your meds. No algorithm can know if you didn’t take it because you were broke, or broken, or just too tired to care.
Maybe the real revolution isn’t in the sensor. It’s in the conversation that follows the alert. If the doctor says, ‘You missed three doses,’ and the patient says, ‘I couldn’t afford my rent this month,’ then we’ve got something real.
Otherwise, we’re just automating guilt.
Lisa Dore
January 6, 2026 AT 07:38Okay, I just told my 70-year-old neighbor about this and she lit up. She’s on five meds and her daughter lives across the country. She said, ‘If I forget, maybe she’ll know before I end up in the hospital.’ That’s the heart of this, right? It’s not about control. It’s about connection. It’s about someone who loves you getting a heads-up before it’s too late.
And yeah, the app’s clunky. But imagine if it had a ‘call my daughter’ button built in? Or a voice note option? ‘Hi, Mom, I took my pill today.’ That’s not surveillance. That’s love with tech.
Let’s not get so scared of the data that we ignore the human need behind it. We’re not just tracking pills-we’re tracking care. And that’s worth fighting for.
Also-can we PLEASE get a version that works without a phone? Like, a little base station that beeps when you take it? My grandma doesn’t own a smartphone. But she has a TV remote. That’s her tech. Let’s meet people where they are.
Sharleen Luciano
January 6, 2026 AT 14:49How quaint. A $100 pill with a sensor that does what? Confirms you swallowed a capsule? That’s not innovation-that’s a gimmick for people who can’t follow basic instructions. And now we’re going to train AI to guess your nausea from your step count? Please. You’re treating physiology like a TikTok trend. The real issue is systemic: poor patient education, fragmented care, and pharmaceutical greed. This tech doesn’t fix any of that. It just makes the problem look like it’s being solved while the actual costs keep rising.
And let’s not pretend this isn’t a revenue stream for Medtronic. You think they’re doing this out of altruism? Please. They’re monetizing your bio-data. The real ‘digital pill’ is your personal health data being sold to the highest bidder. The sensor is just the wrapper.
Jim Rice
January 7, 2026 AT 15:09So if I skip my pill, my doctor gets a notification? And if I’m ‘inactive’ after taking it, they assume I’m ‘experiencing side effects’? That’s not medicine. That’s a prison sentence with a Bluetooth patch. What’s next? Mandatory wearables for people on antidepressants? You think we don’t know what’s happening here? You’re turning compliance into a loyalty program. ‘Good job, Karen, you swallowed your antihypertensive. Here’s a badge.’
And you wonder why people stop taking meds? Because it feels like being watched. Not helped.
Also, ‘AI predicts side effects’? So now my heart rate spike means I’m ‘at risk’? I just ran up the stairs. Chill. You’re pathologizing normal human biology.
This isn’t healthcare. It’s surveillance capitalism with a stethoscope.
Henriette Barrows
January 7, 2026 AT 15:33I’m on a daily antipsychotic and I used the digital pill for six months. Honestly? It saved me. I didn’t realize I was skipping doses on weekends until the log showed it. I thought I was fine. But the data didn’t lie. I started talking to my therapist about why I skipped. Turns out I was scared of the side effects and didn’t know how to talk about it. The sensor didn’t judge me. It just showed me the truth.
And yeah, the app was annoying. But my sister helped me set it up. We made a little ritual: ‘Pill time = tea time.’ It became part of my routine, not a chore.
Privacy? I asked my doctor. They said the data is encrypted, HIPAA-protected, and I can delete it anytime. I did. Twice. I felt in control.
It’s not perfect. But it gave me back my autonomy. That’s worth more than $100.
Alex Ronald
January 9, 2026 AT 03:13For people on TB meds or post-transplant regimens, this isn’t luxury tech-it’s survival. I’ve seen patients die because they missed a dose and no one knew. Digital pills don’t replace human care. They amplify it. When a nurse sees a pattern of skipped doses, she can call, not chastise. That’s the power.
Yes, cost is a barrier. But if we treat this like insulin-essential, life-saving, subsidized-it becomes accessible. We don’t charge extra for insulin sensors. Why should we for digital pills?
And the side effect detection? It’s not magic. But it’s a tool. A simple one. Like a thermometer. If your temp spikes after a med, you know something’s off. Same here.
Let’s stop calling it surveillance. It’s early warning. And for some of us? That’s the only thing standing between life and death.
Teresa Rodriguez leon
January 10, 2026 AT 12:48This is terrifying. I don’t want my heart rate tracked. I don’t want my sleep logged. I don’t want my body turned into a spreadsheet. What happens when the hackers get in? What happens when my employer finds out I was ‘inactive’ for three days after my divorce? I’m not a patient. I’m a person. And I refuse to be monitored like a lab animal. No thank you. I’ll take my chances with forgetfulness.
Manan Pandya
January 12, 2026 AT 11:49Excellent breakdown. The real challenge isn't the technology-it's the cultural gap. We've built a system that rewards compliance over compassion. The sensor can tell us if a pill was swallowed, but it can't tell us why someone felt too exhausted to take it. Or why they couldn't afford the co-pay. Or why they were ashamed to admit they were struggling.
Let’s not mistake data for understanding. The best digital pill system in the world won’t help if the doctor doesn’t listen. The patch is just a mirror. What matters is what we do with the reflection.
Also, for elderly users: a simple voice-activated system that says, ‘Did you take your pill?’ and lets them say ‘yes’ or ‘no’-that’s the real innovation. Not the sensor. The conversation.
Emma Duquemin
January 13, 2026 AT 01:42Wait-I just realized something. We’re all talking about the tech, but no one’s talking about the humans who built it. The engineers who designed the sensor to work in acidic environments. The nurses who called patients when the patch fell off. The coders who made the app voice-friendly. This isn’t just corporate greed. It’s also a bunch of tired, brilliant people trying to fix something broken.
So yeah, the system’s flawed. The cost is insane. The privacy? Still a mess.
But the people? They’re trying. And maybe that’s the real story.
Let’s not hate the tool. Let’s demand better from the people using it.