Drug shortages aren’t just inconveniences-they’re life-threatening. When a critical antibiotic or IV fluid disappears from hospital shelves, doctors scramble. Patients delay treatments. Some die. The problem isn’t random. It’s built into how drugs are made and moved around the world. And it’s getting worse, not better.
More than 245 drug shortages were recorded in the U.S. in 2022 alone. Over half of them involved sterile injectables-medicines used in emergency rooms, ICUs, and operating theaters. These aren’t niche drugs. They’re the backbone of modern care. Yet, the system keeping them available is dangerously fragile. The root cause? A global supply chain designed for cheapness, not safety.
Why the drug supply chain is broken
The modern pharmaceutical supply chain runs on lean principles. Companies cut costs by relying on single suppliers, faraway factories, and just-in-time delivery. It works fine until it doesn’t. When a factory in India shuts down for regulatory issues, or a shipping port in China closes due to political unrest, the ripple effect hits U.S. hospitals within weeks.
Here’s the harsh truth: 72% of the active ingredients (APIs) used in U.S. drugs are made overseas. Nearly 30% of those come from just two countries-China and India. That’s not diversification. That’s concentration. And it’s a single point of failure waiting to happen.
Even worse, most companies don’t even know where their raw materials come from. Only 12% have visibility past three tiers down the supply chain. That means if a chemical supplier in Vietnam has a fire, the manufacturer in Ohio won’t find out until it’s too late. No early warning. No backup plan. Just silence-and then a shortage.
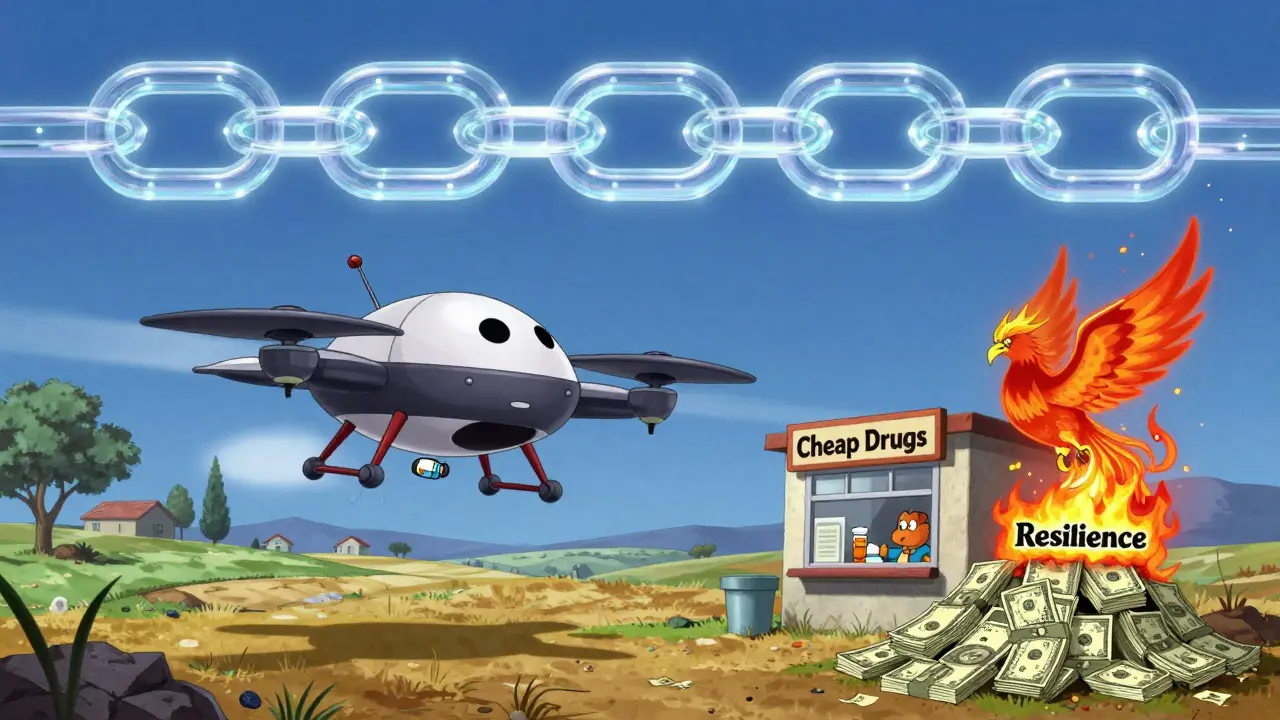
What resilience actually looks like
Building resilience doesn’t mean building more factories. It means redesigning the system so it can bend without breaking. Experts agree on three core capabilities: anticipation, planning, and risk mitigation.
Anticipation means knowing what could go wrong before it happens. That requires real-time data on supplier performance, geopolitical risks, and weather patterns affecting shipping routes. AI tools now predict disruptions with 83% accuracy up to 30 days out. Companies using this tech saw 32% fewer supply issues-even though they spent far less than those relying on old-school methods.
Strategic planning means designing your supply chain like you design a bridge: with backups. The gold standard? Having at least three geographically separate suppliers for every critical drug. For high-risk medicines, manufacturers should dual-source the active ingredient-meaning two factories make the same thing, on different continents. That way, if one fails, the other picks up the slack.
Risk mitigation is about having tools ready when disaster strikes. That includes buffer stockpiles. Experts recommend keeping 6 to 12 months’ worth of critical drugs on hand. Sounds expensive? It is. But it’s cheaper than the alternative. In 2023, drug shortages cost the U.S. healthcare system $216 million in extra expenses-from emergency air shipments to costly substitutes.

The cost of doing nothing
Some argue that building resilience is too expensive. But the real cost isn’t what you spend-it’s what you lose.
Reshoring all API production to the U.S. would raise costs by 25-40%. That’s a lot. But a hybrid model-keeping the most critical drugs made domestically while diversifying others across Asia, Europe, and Latin America-cuts shortages by 85% at just $1.2-1.8 billion a year. Compare that to stockpiling everything: it would cost $3.5-4.2 billion annually and only prevent 45% of shortages.
And then there’s cybersecurity. Between 2020 and 2023, cyberattacks on drug supply chains jumped 214%. Hackers don’t just steal data-they shut down production lines. A single ransomware attack can paralyze a factory for weeks. The solution? Embedding NIST cybersecurity standards into every partner’s operations. It’s not optional anymore.
Real-world examples: who’s getting it right
Pfizer spent $220 million over 18 months to install AI-driven demand forecasting across 150 distribution centers. Result? A 38% drop in stockouts. Merck took $85 million in federal aid to build a new API plant in Pennsylvania for key antibiotics. Now 95% of those drugs are made in the U.S. The cost? 31% higher production. But with adjusted Medicare reimbursements, it’s sustainable.
Even distributors are innovating. One group in the Midwest installed drone delivery networks for rural pharmacies. What used to take 72 hours now takes 4. Regulatory hurdles? Yes. But 42 states are now reviewing the rules.
These aren’t outliers. They’re proof that change is possible. The problem isn’t technology. It’s incentives.
The biggest barrier: money and misaligned incentives
Why aren’t more companies doing this? Because pharmacy buyers still choose the cheapest drug-even if it comes from a single, risky supplier. Procurement departments are judged on cost savings, not supply stability. That’s backward.
Only 35% of pharmaceutical companies have staff trained in supply chain risk analytics. And 78% use incompatible data systems. That means no one talks to each other. No one sees the full picture. No one can act fast enough.
The solution? Change how we pay for drugs. The Centers for Medicare & Medicaid Services (CMS) is proposing a rule that would tie reimbursement to supply chain transparency. By 2026, manufacturers will have to disclose every step of their supply chain-from raw chemical mines to the final pill bottle. If they can’t prove resilience, they won’t get paid.
This is the game-changer. When money follows safety, companies will finally invest in it.
What’s next: policy, tech, and the road to 2030
The FDA now requires annual vulnerability assessments from all drugmakers. Full compliance is due by Q3 2025. The European Medicines Agency is doing the same. And the U.S. government is spending $520 million to boost domestic production of 50 critical drugs, aiming for 40% API manufacturing onshore by 2027.
Meanwhile, AI adoption in supply chains has jumped from 22% in 2021 to 58% in 2023. Predictive models are getting smarter. Blockchain is being tested for real-time tracking. And venture capital poured $2.3 billion into supply chain visibility startups last year alone.
By 2030, experts predict comprehensive resilience measures could cut critical drug shortages by 75%. But it won’t happen without sustained investment-$2.1 to $3.4 billion a year. That’s just 0.3% of total U.S. prescription drug spending. A small price to pay for never having to choose which patient gets the last dose.
The system was built to save money. It’s time to rebuild it to save lives.


Elan Ricarte
February 8, 2026 AT 11:26Susan Kwan
February 9, 2026 AT 18:34Frank Baumann
February 11, 2026 AT 04:13Ritteka Goyal
February 13, 2026 AT 03:23Ryan Vargas
February 14, 2026 AT 20:40Chelsea Deflyss
February 15, 2026 AT 11:11Brett Pouser
February 16, 2026 AT 07:04Tasha Lake
February 16, 2026 AT 23:45Sam Dickison
February 17, 2026 AT 14:37MANI V
February 18, 2026 AT 10:56Angie Datuin
February 18, 2026 AT 22:29Random Guy
February 19, 2026 AT 00:26