Most people with cirrhosis don’t know they’re at high risk for liver cancer-until it’s too late. Hepatocellular carcinoma (HCC) is the most common type of liver cancer, and over 80% of cases happen in people who already have cirrhosis. The good news? If caught early, HCC can often be cured. The bad news? Most cases are found too late because surveillance isn’t happening as it should.
Why Surveillance Matters for People with Cirrhosis
If you have cirrhosis, your liver is scarred. That scarring doesn’t just slow down liver function-it creates the perfect environment for cancer to grow. HCC doesn’t show symptoms in its early stages. By the time someone feels pain, loses weight, or turns yellow, the tumor is often too large to remove. That’s why screening isn’t optional-it’s life-saving. Studies show that people who get regular surveillance live longer. Without it, only 10-20% survive five years after diagnosis. With it, that number jumps to 50-70%. One major study found that regular screening added about three months to life expectancy for people with a 1.5% annual risk of HCC. That might not sound like much, but when you’re talking about cancer, those months matter.What Does HCC Surveillance Actually Look Like?
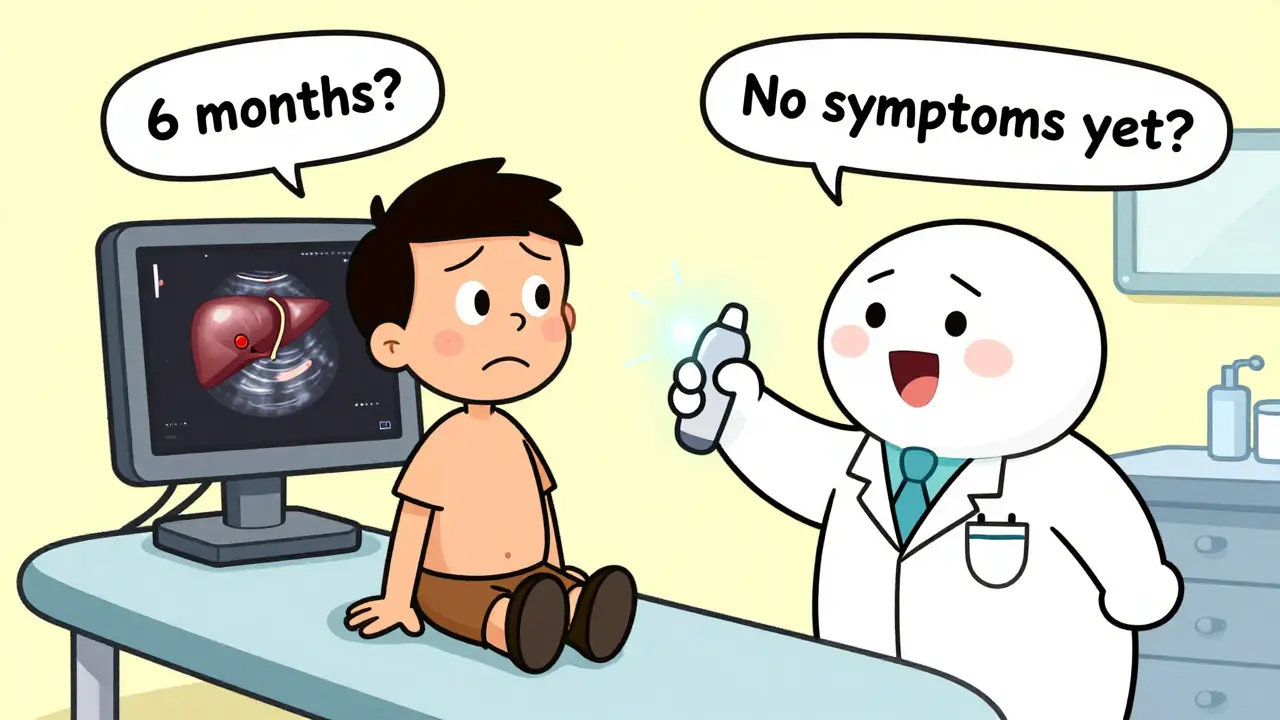
The standard screening test is a liver ultrasound every six months. It’s simple, non-invasive, and doesn’t use radiation. A technician moves a probe over your abdomen to look for lumps or abnormal areas. If something suspicious shows up, you’ll need a more detailed scan-usually an MRI or contrast-enhanced CT. Some guidelines also suggest checking a blood marker called alpha-fetoprotein (AFP). But AFP isn’t perfect. It can be high for reasons other than cancer, like active hepatitis. And many early HCC tumors don’t raise AFP at all. So while some doctors still order it, most experts now say ultrasound alone is enough. If AFP is above 20 ng/mL, that’s a red flag-but it doesn’t replace imaging. The timing matters too. HCC tumors grow about 1-2 cm every six months in cirrhotic livers. That’s why screening every six months is the sweet spot. Screen too early, and you waste resources. Screen too late, and you miss the window for cure.Who Should Be Screened? Not Everyone with Cirrhosis
For years, the rule was simple: if you have cirrhosis, you get screened. But that’s changing. New research shows not all cirrhosis is the same. Your risk depends on what caused it, how advanced it is, and your overall health. The European Association for the Study of the Liver (EASL) now recommends risk-based screening. They divide cirrhosis patients into three groups:- High risk (over 2.5% annual risk): Ultrasound every six months, or possibly MRI.
- Medium risk (1.5-2.5% annual risk): Standard six-month ultrasound.
- Low risk (under 1.5% annual risk): Screening may not be needed.
What Happens If Something Is Found?
If your ultrasound shows a mass larger than 1 cm, you don’t wait. You go straight to a multiphase MRI or CT scan. These scans use contrast dye to see how the tumor takes up blood-something HCC does differently than benign lumps. Radiologists use a system called LI-RADS (Liver Imaging Reporting and Data System) to classify what they see. It’s like a traffic light: LR-1 is definitely benign, LR-5 is definitely HCC, and LR-3 or LR-4 means it’s probably cancer but needs more testing. If the diagnosis is confirmed, treatment depends on how far the cancer has spread and how well your liver still works. The Barcelona Clinic Liver Cancer (BCLC) staging system is used worldwide to guide choices.Treatment Options: From Cure to Control
If HCC is caught early (BCLC stage 0 or A), you have a real shot at cure:- Surgical removal: Removing the tumor is possible if it’s small and your liver is still functioning well.
- Liver transplant: The best option for many. You get a new liver and the cancer is gone. But you need to meet strict criteria-usually one tumor under 5 cm or up to three tumors under 3 cm each.
- Radiofrequency ablation (RFA): A needle is inserted into the tumor through the skin. Heat destroys the cancer cells. It’s used for tumors under 3 cm.
- Targeted drugs: Sorafenib and lenvatinib are oral pills that block signals cancer cells use to grow. They can extend life by several months.
- Immunotherapy: Drugs like nivolumab and pembrolizumab help your immune system recognize and attack cancer. They’re now used in combination with other drugs for advanced HCC.
- Clinical trials: New treatments are being tested all the time. If you’re eligible, it’s worth asking about.
Why Is Surveillance So Poorly Done?
Even though guidelines are clear, only 30-50% of cirrhotic patients in the U.S. get screened regularly. Why?- Doctors don’t know: Many primary care providers aren’t trained to recognize who needs screening. Cirrhosis is often managed by specialists, but follow-up care falls to general doctors.
- No reminders: In 67% of clinics, there’s no electronic alert in the medical record when a patient with cirrhosis is due for a scan.
- Patient barriers: People miss appointments due to transportation, work, or fear. One study found 25-40% of patients skip their screening.
- Cost and access: Ultrasound isn’t free. In the U.S., the average cost per year is $287 for ultrasound alone. For patients on Medicaid, it’s harder to get scheduled.
- Racial disparities: White patients are 50% more likely to get screened than Black patients. Insurance status makes a big difference too.
What’s Changing in 2025 and Beyond?
The field is moving fast. New tools are emerging:- AI-assisted ultrasound: Tools like Medtronic’s LiverAssist help technicians spot tiny tumors that the human eye might miss. They improve detection by up to 22%.
- Better blood tests: The GALAD score combines age, gender, AFP, AFP-L3, and DCP. It detects early HCC with 85% accuracy-better than AFP alone.
- Abbreviated MRI: A 5-7 minute liver MRI now costs $350-400. It’s being studied as a replacement for ultrasound in high-risk patients.
- Risk scores: The aMAP score (based on age, gender, albumin, bilirubin, platelets) can predict risk with 81% accuracy. It’s already being used in some European clinics.
What You Can Do
If you have cirrhosis:- Ask your doctor: “Am I at risk for liver cancer? Should I be screened?”
- Make sure your ultrasound is scheduled every six months. Set a phone reminder.
- If you’re told you don’t need screening, ask why. Get the risk calculation-if your annual risk is over 1.5%, you should be screened.
- Know your liver function. Ask for your Child-Pugh score. If you’re Class C, ask if transplant is an option.
- Don’t wait for symptoms. By then, it’s often too late.
Final Thoughts
Hepatocellular carcinoma doesn’t have to be a death sentence. But it won’t be caught by accident. It needs a system-regular scans, clear protocols, and patients who know their risk. Right now, that system is broken for too many people. The science is solid. The tools are here. What’s missing is consistent action. If you have cirrhosis, don’t assume someone else is watching out for you. Be your own advocate. Ask for the scan. Push for the follow-up. Because in this case, early detection isn’t just helpful-it’s the difference between life and death.Is hepatocellular carcinoma the same as liver cancer?
Yes, hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, making up 75-85% of all cases. Other types exist, like cholangiocarcinoma (bile duct cancer), but when doctors say "liver cancer," they usually mean HCC, especially in people with cirrhosis.
Can you survive hepatocellular carcinoma?
Yes-if it’s caught early. If HCC is found at stage 0 or A, survival rates jump to 50-70% over five years. Treatments like surgery, transplant, or ablation can cure it. But if it’s found late, survival drops to under 20%. That’s why surveillance is critical.
How often should you get screened for HCC if you have cirrhosis?
Every six months. That’s the standard recommendation from major liver societies. Screening too often wastes resources; screening less often misses tumors while they’re still small and treatable. Ultrasound is the go-to test, and it’s done every six months regardless of what caused the cirrhosis-unless your risk is very low.
Do all cirrhosis patients need HCC screening?
Not necessarily. New guidelines suggest screening only if your annual risk is 1.5% or higher. People with advanced liver failure (Child-Pugh Class C) and short life expectancy usually don’t benefit. But most patients with compensated cirrhosis-especially from hepatitis B, hepatitis C after cure, or heavy alcohol use-should be screened.
Can a blood test alone detect liver cancer?
No. The AFP blood test is sometimes used, but it’s unreliable. Many early HCC tumors don’t raise AFP, and other conditions like hepatitis can raise it too. Imaging-ultrasound, MRI, or CT-is required to confirm a diagnosis. Blood tests are only a supplement, not a replacement.
What’s the difference between ultrasound and MRI for HCC screening?
Ultrasound is cheaper, widely available, and used for routine screening. MRI is more sensitive and better at confirming whether a lump is cancer. MRI is used for follow-up after an abnormal ultrasound, or for high-risk patients where even small tumors matter. New abbreviated MRI protocols are making it faster and more affordable-so it may replace ultrasound for some patients in the future.
Is liver cancer screening covered by insurance?
In the U.S., Medicare and most private insurers cover biannual ultrasound for patients with cirrhosis because it’s recommended by major medical societies. Medicaid coverage varies by state. Always check with your provider. If you’re denied, ask for a letter of medical necessity from your hepatologist.
Can you prevent hepatocellular carcinoma?
You can’t always prevent it, but you can reduce your risk. If you have cirrhosis, avoid alcohol completely. Get vaccinated for hepatitis B if you haven’t already. Treat hepatitis C if you have it-curing it lowers but doesn’t eliminate HCC risk. Maintain a healthy weight and control diabetes. And most importantly: get screened regularly.

Nick Cole
January 17, 2026 AT 00:56Man, I wish my dad’s hepatologist had told him about this six months ago. He just got diagnosed with stage B HCC last week-screening was never mentioned during his cirrhosis checkups. This post is a wake-up call for anyone with liver disease.
vivek kumar
January 18, 2026 AT 12:29Let’s be real-80% of HCC cases occur in cirrhotic patients, yet primary care docs treat cirrhosis like it’s just ‘bad liver’ and move on. No alerts, no follow-ups, no urgency. It’s systemic neglect wrapped in medical jargon. We need mandatory EHR triggers for cirrhosis patients. Not optional. Mandatory.
Riya Katyal
January 19, 2026 AT 02:03Oh wow, so we’re supposed to trust ultrasound? The same tech that missed my cousin’s ovarian tumor ‘because it was hiding behind her bladder’? 🙄 Maybe we should just start with MRI for everyone and skip the ‘maybe it’s nothing’ dance.
waneta rozwan
January 20, 2026 AT 07:50Y’all are missing the point. This isn’t about scans or blood tests-it’s about how medicine treats poor people. If you’re on Medicaid in Alabama, you wait 11 weeks for an ultrasound. If you’re a white guy in Boston with private insurance? You get it next Tuesday. This is healthcare apartheid, and no algorithm fixes that.
Nicholas Gabriel
January 21, 2026 AT 12:34Just to clarify: AFP is not a reliable standalone test, and LI-RADS is the gold standard for imaging interpretation-but only if the radiologist is trained in it. Many community hospitals still use outdated criteria. Also, the aMAP score? It’s validated in 12 countries. Why aren’t we using it in the U.S.? We’re still stuck in 2010.
Cheryl Griffith
January 22, 2026 AT 09:50I’m a nurse who works in hepatology, and I’ve seen this play out too many times. Patients come in scared, confused, and exhausted. They don’t know their Child-Pugh score. They’ve never heard of TACE. And when we explain it, they nod politely-but they don’t believe it’ll help. We need better education, not just better scans.
swarnima singh
January 24, 2026 AT 01:25so like… if u have cirrhosis from drinking and then stop… is ur risk still high? or is it like… u just get a free pass? bc i know this guy who quit drinking 7 years ago and still gets yelled at by his doc to get ultrasounds… like… bro i’m clean now???
Isabella Reid
January 25, 2026 AT 12:27My aunt in India got her first ultrasound at 72 after collapsing. Turns out she had HCC for 18 months. No one ever told her to get screened-even though she had hepatitis B for 30 years. This isn’t just a U.S. problem. It’s global. We need low-cost, community-based screening programs. Not just fancy AI tools in academic centers.
Jody Fahrenkrug
January 25, 2026 AT 17:34My mom had cirrhosis from NASH. We scheduled her ultrasound every six months like clockwork. One time, the tech said, ‘This looks weird.’ Turned out it was a 1.2 cm tumor. We caught it early. She had RFA. No transplant. No chemo. Just a needle and a miracle. Don’t skip your scan. Seriously.
Samyak Shertok
January 27, 2026 AT 08:52Ohhh so now we’re gonna use AI to fix the fact that doctors don’t care? Cool. Next they’ll use a chatbot to tell people to stop drinking. Let me guess-the real solution is just to make cirrhosis patients pay more for insurance so they ‘learn responsibility.’ 😌
Stephen Tulloch
January 28, 2026 AT 14:24Bro, if you’re not getting an abbreviated MRI every 6 months and you have cirrhosis, you’re basically gambling with your liver. Like, ultrasound is fine for grandma in 2008-but we got AI + contrast-enhanced MRI now. Stop living in the past. 🚀🩺
Joie Cregin
January 29, 2026 AT 01:48My best friend’s dad died of HCC last year. He was a retired firefighter-healthy, active, never touched alcohol. Got cirrhosis from undiagnosed hepatitis C. They found the tumor during a routine blood draw-because his doctor finally ordered an AFP after he lost 20 pounds. Too late. I’m telling everyone I know: if you’ve got cirrhosis, be the annoying one who asks for the scan. Again. And again. And again.