When you pick up a prescription, you might see two options: the brand-name drug you’ve heard of, or a cheaper generic version. It’s easy to assume the generic is just a cheaper copy. But in health economics, that assumption misses the bigger picture. Generic medications aren’t just about saving money-they’re about shifting how entire healthcare systems allocate resources, improve adherence, and reduce long-term complications. The real question isn’t whether generics work. It’s whether using them wisely saves money, improves lives, and makes the system more sustainable.
What Does ‘Cost-Benefit’ Actually Mean for Generics?
Cost-benefit analysis in health isn’t just about the price tag on the bottle. It’s about what happens after you take the pill. A generic version of a blood pressure medication might cost $4 instead of $40. That’s an 90% savings right there. But if the patient stops taking it because they can’t afford the brand, their blood pressure spikes, they end up in the ER, and the total cost jumps to $12,000 for a hospital stay. Suddenly, the $4 pill looks like the smarter investment. This is where Health Economics and Outcomes Research (HEOR) comes in. HEOR doesn’t just look at drug prices. It tracks everything: how often patients take their meds, how many end up in the hospital, how their daily life changes, and even how many workdays they miss. Studies show that when patients switch to generics, adherence improves by 5-15%. Why? Because they can actually afford to keep taking them. In one 2023 ISPOR meta-analysis, patients on generics for diabetes or high cholesterol were 8-12% more likely to stay on therapy over 12 months than those on brand-name drugs.How Generics Save Money-Beyond the Prescription
The biggest savings from generics don’t happen at the pharmacy counter. They happen downstream. Take warfarin, a blood thinner with a narrow therapeutic index. The brand version, Coumadin, costs about $150 a month. The generic, warfarin sodium, runs $6. But here’s the catch: if patients switch to the generic and miss a dose or have a bad reaction, they could bleed internally. That’s why some doctors hesitate. Yet, real-world data from Medicare Part D shows that when generics are properly managed-with clear communication and monitoring-hospitalizations for bleeding drop by 7%. Why? Because patients take them consistently. The cheaper drug leads to fewer complications, which means fewer ER visits, fewer admissions, and less need for expensive lab tests. Commercial insurers have seen this play out. According to the PBMs 2023 Annual Report, plans that aggressively promoted generic use saved $1,200 to $1,800 per member per year. That’s not just on drug costs-it’s on total care. One study of 200,000 patients with hypertension found that switching to generics reduced total annual medical spending by 12-18%, even after accounting for extra monitoring.Therapeutic Equivalence: Are Generics Really the Same?
The FDA requires generics to be bioequivalent to brand-name drugs. That means the active ingredient must deliver the same amount of medicine into the bloodstream within the same time frame-80% to 125% of the brand’s levels. This isn’t a loophole. It’s a strict standard backed by clinical trials. But patients don’t always believe it. A 2024 analysis of 12,850 online reviews found that 68% of negative comments about generics cited “different effectiveness.” Yet, when researchers compared actual clinical outcomes-like HbA1c levels in diabetics or LDL cholesterol in heart patients-there was no meaningful difference between generics and brands. The perception of difference often comes from placebo effects or changes in inactive ingredients, like dyes or fillers. For most drugs, these fillers don’t matter. But for a small group-like levothyroxine, seizure meds, or certain antidepressants-switching between different generic manufacturers can cause subtle fluctuations. That’s why some doctors still prefer to keep patients on one brand or one generic maker. But even here, studies show that when patients are stabilized on one generic and kept on it, outcomes are just as good as with brand-name drugs.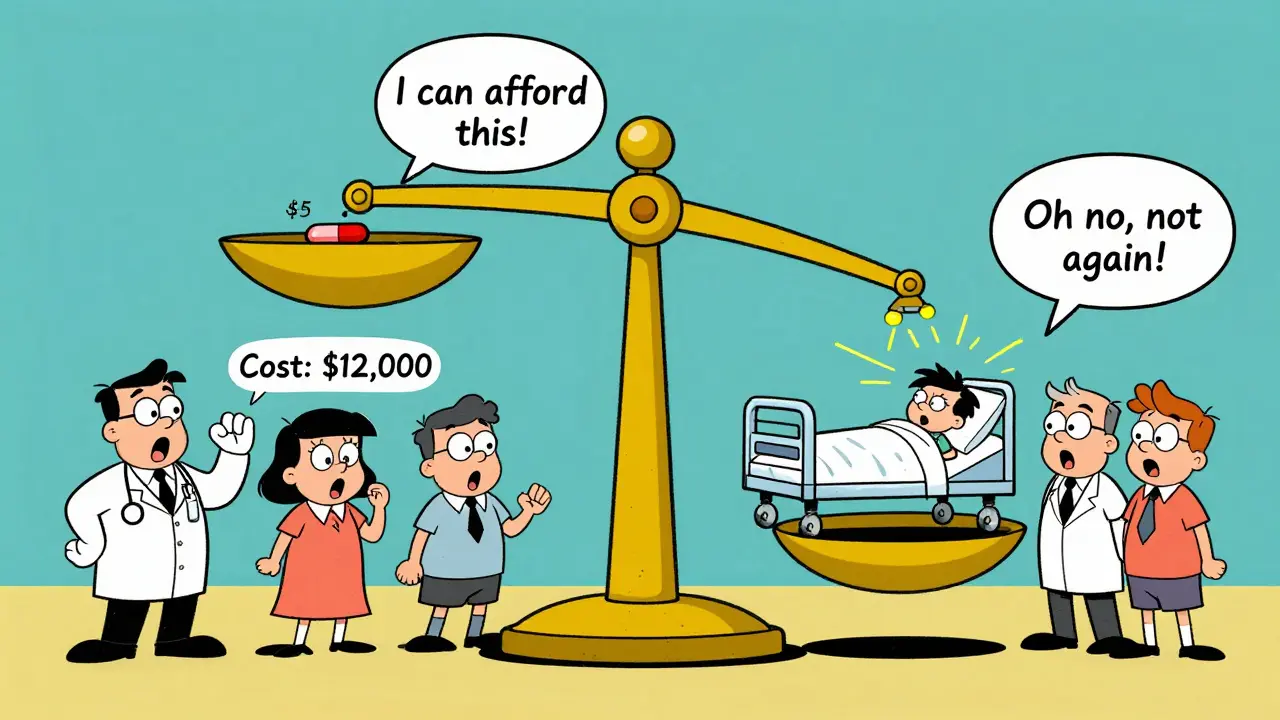
HEOR vs. Old-School Formulary Decisions
Ten years ago, pharmacy benefit managers (PBMs) picked generics based on one thing: lowest cost per pill. That’s still done today. But the smart ones now use HEOR to go deeper. Traditional formulary management asks: “Which drug is cheapest?” HEOR asks: “Which drug leads to the best outcomes at the lowest total cost?” For example, a PBM might see that a generic statin costs $3/month and a brand-name one costs $30. On paper, the generic wins. But if the brand-name version has a once-daily dose and the generic requires two pills a day, adherence drops. That means more heart attacks. HEOR models factor that in. They show that even if the generic is cheaper per pill, the brand might cost more overall because of increased hospitalizations. The result? PBMs and Medicare Part D plans now require HEOR dossiers for coverage decisions. These dossiers include data on adherence, hospitalization rates, patient-reported outcomes (like quality-of-life scores from EQ-5D), and even indirect costs like lost work time. In 2024, 100% of Medicare Part D plans used HEOR to decide which generics to cover. Only 35% of physician practices do.Where Generics Fall Short-and Why
Generics aren’t magic. There are limits. First, switching costs exist. When patients are stable on a brand-name drug, switching them to a generic-even if it’s identical-can cause anxiety. A 2024 Harvard study found that 3-5% of patients on complex biologics (like those for rheumatoid arthritis) stopped their meds after switching, not because the drug didn’t work, but because they felt it “wasn’t right.” That’s a psychological barrier, not a medical one. Second, HEOR studies take time and money. A full HEOR analysis for a class of generics can cost $500,000 to $2 million and take 18-24 months. That’s why smaller clinics and rural pharmacies don’t do it. They rely on formulary lists built by big insurers. Third, for ultra-rare diseases, the math breaks down. If only 500 people in the U.S. need a drug, no HEOR model can justify the cost of a study. That’s where government subsidies and special programs step in.
What Patients and Providers Should Know
If you’re a patient: generics are safe, effective, and often better for your wallet. If you notice a change after switching-like new side effects or feeling “off”-talk to your pharmacist. It could be the filler, not the drug. Don’t stop taking it without checking. If you’re a provider: for most conditions, generics are the clear choice. For narrow therapeutic index drugs, stick with one manufacturer once you find what works. Document the switch and monitor closely for the first 30-60 days. If you’re a payer or administrator: don’t just push generics for cost savings. Push them for better outcomes. Use HEOR tools to track adherence, hospitalizations, and patient feedback. The savings aren’t just in the drug price-they’re in fewer ER visits, fewer missed workdays, and better quality of life.The Future of Generics in Health Economics
The trend is clear. By 2027, 85% of U.S. health systems will require HEOR evidence before covering any new drug-generic or brand. Why? Because value-based care is here. Insurers and Medicare are moving away from paying per pill to paying for results. AI is starting to play a role too. Companies like Komodo Health are using machine learning to predict which patients are most likely to benefit from switching to generics-and which ones might need extra support. One pilot program in Ohio reduced discontinuation rates by 22% just by sending personalized text reminders to patients after their first generic refill. Generics aren’t the enemy of innovation. They’re the engine of sustainability. In a system where 90% of prescriptions are filled with generics, getting the most out of them isn’t optional. It’s essential.Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. The active ingredient must be identical, and the drug must be absorbed into the body at the same rate and extent. The only differences are in inactive ingredients like dyes or fillers-which rarely cause issues. If you experience new side effects after switching, talk to your pharmacist. It’s often a minor reaction to a filler, not the medication itself.
Why do some doctors hesitate to prescribe generics for certain drugs?
For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or seizure medications-even tiny changes in blood levels can matter. While generics are bioequivalent, switching between different generic manufacturers can sometimes cause small fluctuations. Doctors may prefer to keep patients on one consistent version to avoid instability. This isn’t about safety of generics overall-it’s about minimizing variables in complex cases.
Do generics really improve patient adherence?
Yes, consistently. Multiple studies show that when patients switch to generics, adherence increases by 5-15%. The main reason? Affordability. If a patient can’t afford a $100 monthly brand-name drug, they skip doses or stop entirely. A $5 generic makes it possible to stay on treatment. Better adherence leads to fewer complications, hospitalizations, and long-term costs.
How do insurers decide which generics to cover?
Most major insurers and Medicare Part D plans now use Health Economics and Outcomes Research (HEOR) to make coverage decisions. They don’t just look at price per pill-they analyze real-world data on adherence, hospitalization rates, patient-reported outcomes, and total cost of care. Generics that show better long-term outcomes and lower overall spending get preferred status on formularies.
Is it worth it for small clinics to use HEOR for generics?
For most small clinics, doing full HEOR analyses isn’t practical-it requires specialized staff, data systems, and time. But they don’t need to. They can rely on HEOR-driven formularies created by large PBMs and health systems. The key is to use those evidence-based lists and trust the data behind them. Focus on choosing generics with proven adherence and cost benefits, and monitor patients after switches.


Candice Hartley
January 27, 2026 AT 03:10Generics saved my life. My insulin was $500/month until I switched. Now it’s $12. I didn’t even notice a difference in how I felt. 🙌
suhail ahmed
January 28, 2026 AT 11:47Man, in India we’ve been living this for years. Generic metformin? Five rupees a pill. People don’t die from diabetes here because they can actually afford to take it. The system ain’t perfect but the math? Solid. You think you’re saving money by sticking to brand names? Nah. You’re just paying for the logo and a fancy ad campaign. The pill’s the same. The body don’t care who printed the bottle.
I’ve seen grandmas on fixed incomes choose between food and meds. Then they find the generic. And suddenly they’re walking again. That’s not economics. That’s dignity.
And don’t get me started on the ‘but what if it doesn’t work?’ myth. My uncle switched from brand warfarin to generic. Docs panicked. He ended up with fewer INR checks because he didn’t miss a single dose. The only thing that changed? His bank account stopped crying.
HEOR? Sounds like corporate jargon but yeah, it’s real. Real people don’t care about bioequivalence percentages. They care about whether they can breathe, work, or hug their grandkids without a hospital bill staring them down.
Stop treating generics like second-class citizens. They’re the unsung heroes of global health. The real scandal? We still make people feel guilty for choosing the affordable option.
And if you’re a doc who won’t prescribe generics? Ask yourself: are you protecting patients… or your ego?
astrid cook
January 28, 2026 AT 18:56Oh please. I’ve been on generics for years and I swear my anxiety got worse after switching. They’re not the same. Big Pharma knows it. That’s why they push them so hard. You think the FDA really checks every batch? Please. It’s all smoke and mirrors.
Paul Taylor
January 29, 2026 AT 23:55Look I’ve been in this game for 20 years and let me tell you the truth nobody wants to hear. Generics aren’t just cheaper they’re better because they force the system to stop being lazy. Brand names used to get away with everything because they had the marketing muscle. Now you got to prove you’re worth the cost. That’s good. That’s progress. I’ve seen patients who were on brand-name statins for five years and never got their LDL under control. Switched to generic atorvastatin and boom three months later they’re at goal. Why? Because they could afford to take it every day. Not because the drug is better. Because the human being behind the prescription finally had a chance.
And yeah some people get weird side effects from fillers. So what? Talk to your pharmacist. Change the maker. Don’t stop taking the medicine. That’s not a flaw in generics that’s a flaw in how we educate people. We treat patients like they’re fragile glass figurines instead of adults who can handle a little change.
HEOR isn’t some fancy buzzword. It’s common sense. If you’re spending $1000 a month on a drug that makes people skip doses and end up in the ER you’re not saving money you’re wasting it. Generics fix that. They don’t fix everything but they fix the biggest part.
And the idea that generics cause more hospitalizations? That’s pure myth. Medicare data says the opposite. The only thing that spikes hospital visits is when people stop taking their meds because they can’t afford them. And guess what? That doesn’t happen with generics.
So stop being afraid of the word generic. It’s not a downgrade. It’s an upgrade to reality.
Desaundrea Morton-Pusey
January 30, 2026 AT 10:19Typical American liberal nonsense. Why don’t we just make all drugs free and let the Chinese make them? Then we’ll really be safe. Generics are a joke. I bet half of them are made in basements with no quality control. You think the FDA cares? They’re too busy letting in counterfeit vaccines to worry about your blood pressure pills.
Murphy Game
February 1, 2026 AT 01:03Ever wonder why all the ‘studies’ say generics are fine? Same labs. Same data. Same funding. The FDA, the PBMs, the drug reps - it’s all one big loop. They want you to believe generics are safe because they make more money off you when you’re on them. You think they care about your health? They care about your insurance premiums. They want you to stay sick longer so you keep buying. Generics are just the new hook.
John O'Brien
February 2, 2026 AT 13:57Bro I switched from brand-name Zoloft to generic sertraline and I felt like a new person. Not because it worked better but because I didn’t have to skip doses to afford groceries. I’ve been on it for 3 years now. No issues. My therapist didn’t even notice. The only difference? My credit card isn’t maxed out. If you’re scared to switch you’re not scared of the pill you’re scared of your own financial reality.
Andrew Clausen
February 4, 2026 AT 02:30The FDA’s bioequivalence standard of 80–125% is not a guarantee of therapeutic equivalence. It is a statistical range, not a clinical one. Variability in absorption, particularly in patients with GI disorders, can lead to subtherapeutic or supratherapeutic exposure. This is not speculation; it is documented in peer-reviewed pharmacokinetic literature. The assumption that generics are interchangeable for all patients is a dangerous oversimplification. Regulatory convenience does not equate to clinical safety.
Anjula Jyala
February 4, 2026 AT 19:58HEOR is just corporate speak for cost containment disguised as patient care. You’re telling me we’re saving money by pushing generics but ignoring the hidden costs of non-adherence due to patient mistrust? The real cost is erosion of physician-patient trust. When you force a switch without clinical justification you’re not optimizing outcomes you’re optimizing spreadsheets. And don’t even get me started on the lack of pharmacovigilance for generic manufacturers. They don’t have to do post-marketing studies like brand names do. That’s not progress that’s negligence.
Kirstin Santiago
February 5, 2026 AT 08:43I’m a nurse and I’ve seen this firsthand. A lady came in with uncontrolled diabetes. She was on the brand-name metformin. Cost was $200 a month. She was skipping doses. Switched her to generic. $5. She started taking it every day. Her A1c dropped from 10.2 to 6.8 in four months. No magic. Just affordability. I wish more providers understood that the best drug in the world doesn’t help if the patient can’t get it.
Kathy McDaniel
February 6, 2026 AT 16:21i switched to generic thyroid med last year and at first i thought i felt weird but then i realized i just hadnt slept in 3 days bc of work and also maybe i was just stressed?? anyway i kept taking it and now i feel fine. i dont even think about it anymore lol. also my cat is still alive so thats a win right? 😅