When you start getting winded climbing stairs-or even walking to the mailbox-and your doctor keeps saying it’s just aging or asthma, but you know something’s off, that’s often the first red flag of pulmonary hypertension. It doesn’t shout. It whispers. By the time the symptoms are obvious, the right side of your heart is already struggling. And if it’s not caught early, that strain can become permanent.
What Pulmonary Hypertension Really Means
Pulmonary hypertension (PH) isn’t just high blood pressure in the lungs. It’s when the arteries carrying blood from your heart to your lungs become stiff, narrow, or blocked. That forces your right ventricle to pump harder just to get blood through. Over time, that extra work thickens the muscle, stretches the chamber, and eventually weakens it. This is right heart strain-and it’s the main reason PH becomes life-threatening.
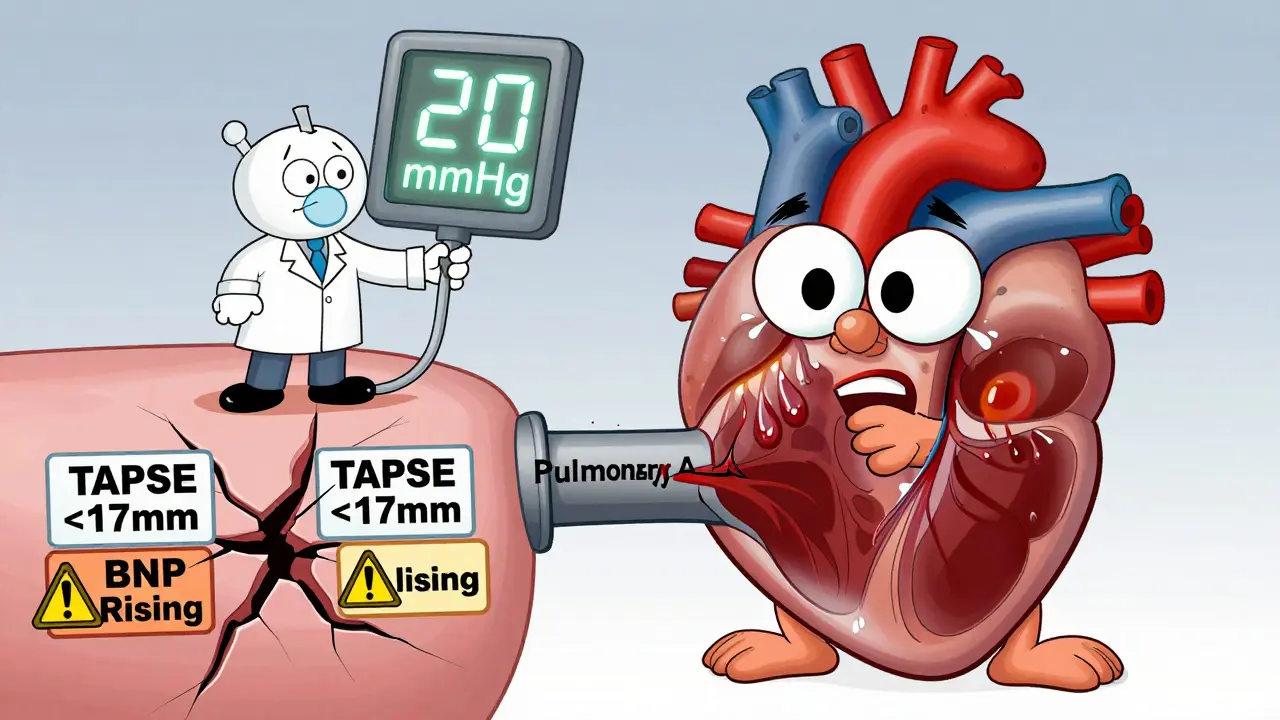
The official diagnosis isn’t based on symptoms alone. It requires a right heart catheterization, where a thin tube is threaded into the pulmonary artery to measure pressure directly. The threshold changed in 2022: now, a mean pulmonary arterial pressure above 20 mmHg at rest counts as PH. Before that, it was 25 mmHg. That small change means more people are being diagnosed earlier, before their hearts are badly damaged.
How Your Body Shows You Something’s Wrong
Early symptoms are easy to ignore. You’re tired. You’re out of shape. Maybe you’re stressed. But here’s what to watch for:
- Shortness of breath during light activity-walking, showering, even talking
- Unexplained fatigue that doesn’t improve with rest
- Swelling in your ankles, legs, or abdomen
- Chest pain or pressure, especially when active
- Dizziness or fainting spells
- A bluish tint to your lips or fingers (cyanosis)
These aren’t normal signs of getting older. In fact, the average person waits nearly three years before getting a correct diagnosis. Many are told they have asthma, COPD, or anxiety. A 2023 survey by the Pulmonary Hypertension Association found 78% of patients were misdiagnosed at first. That delay costs lives.
Right Heart Strain: The Silent Consequence
The right ventricle isn’t built for high pressure. It’s a thin-walled pump designed for low resistance. When the pulmonary arteries stiffen, that chamber starts to remodel. It thickens, enlarges, and loses its ability to contract efficiently. That’s right heart strain.
Doctors look for three key signs on echocardiograms:
- Right ventricular wall thickness over 5 mm
- Right ventricular end-diastolic area larger than 22 cm²
- TAPSE (tricuspid annular plane systolic excursion) under 17 mm
TAPSE is especially telling. If it’s low, your right ventricle isn’t pumping blood out effectively. A TAPSE under 15 mm means you’re at high risk for worsening heart failure. And if your 6-minute walk distance drops below 380 meters, your risk of death in the next year doubles.
Biomarkers like BNP and NT-proBNP rise as the heart stretches. Levels above 180 pg/mL and 1,400 pg/mL, respectively, are strong predictors of poor outcomes. These aren’t just numbers-they’re warning lights.
How Doctors Diagnose It (and Why It’s Hard)
Echocardiograms are the first step. They’re non-invasive, widely available, and can estimate pulmonary pressure. But they’re not perfect. Studies show they overestimate pressure by 10-15 mmHg in nearly half the cases. That means some people get labeled with PH when they don’t have it-and others are missed entirely.
That’s why right heart catheterization remains the gold standard. It’s the only way to confirm the diagnosis and tell the difference between Group 1 PH (pulmonary arterial hypertension) and Group 2 PH (caused by left heart failure). The latter is more common but often overlooked. Dr. Stuart Rich from the University of Chicago found that 30% of Group 2 cases were missed because doctors assumed the high pressure was from the lungs, not the heart.
Cardiac MRI gives the clearest picture of right ventricular size and function, but it’s only available in about one-third of specialized centers. Most clinics rely on echo and catheterization together. And even then, it takes experience. The American Society of Echocardiography says it takes about 120 supervised studies before a technician can reliably spot PH on an echo.
Modern Therapy: From One Drug to Three
Twenty years ago, PH treatment was limited. Most patients got just one drug-often a calcium channel blocker. Survival was measured in months. Today, we have 14 FDA-approved medications across five classes:
- Endothelin receptor antagonists (like bosentan, macitentan)
- PDE-5 inhibitors (sildenafil, tadalafil)
- Prostacyclin analogs (epoprostenol, treprostinil)
- Soluble guanylate cyclase stimulators (riociguat)
- Calcium channel blockers (only for a small subset)
The big shift? Combination therapy. In 2023, 68% of PAH patients started on two or more drugs at once. That’s up from under 20% in 2010. Why? Because PH attacks the body through multiple pathways. Hitting just one doesn’t cut it anymore.
The most exciting new drug is sotatercept. Approved by the FDA in 2021, it targets the TGF-β pathway, which drives artery thickening. In the STELLAR trial, it cut the risk of death or clinical worsening by 44%. It’s not a cure-but it’s the first drug that actually reverses some of the damage.
Why Specialized Centers Matter
PH care isn’t something your local cardiologist can handle alone. It needs a team: a pulmonologist, a heart failure specialist, a pharmacist trained in complex infusions, a nurse coordinator, and sometimes a social worker to help with insurance.
There are only about 35 specialized PH centers in the U.S. Out of 1,000+ hospitals, that’s less than 0.01%. But they treat 75% of patients-and they make a huge difference. The COMPERA registry showed patients under coordinated care had 27% fewer hospitalizations.
Why? Because they catch problems early. A nurse coordinator might notice your BNP is creeping up before you feel worse. They adjust your meds. They check your TAPSE. They make sure your oxygen is optimized. That’s what keeps you out of the ER.

The Real Barriers: Cost, Delay, and Inequality
Even with better treatments, access is uneven. Prostacyclin therapies require continuous IV infusions through a central line and specialized pumps. These cost over $100,000 a year. Insurance companies often delay approval for more than 30 days. A 2023 survey found 63% of patients faced these delays.
And it’s worse for minority populations. A 2023 AHRQ report showed Black and Hispanic patients waited 47% longer for diagnosis than white patients. That delay leads to 32% higher mortality. The Pulmonary Hypertension Association’s 2025 plan is pushing to train primary care doctors to spot the red flags: progressive breathlessness that doesn’t match lung function, unexplained right heart enlargement on EKG, and swelling without heart failure.
What You Can Do
If you’ve been told you’re just “out of shape” but you’re still tired, swollen, or short of breath after minimal effort-push back. Ask for an echocardiogram. Ask if your right heart looks strained. Ask if your BNP has been checked.
If you’re already diagnosed: track your walk distance. Keep a log of your symptoms. Know your numbers-BNP, TAPSE, 6MWD. Don’t wait for your next appointment if you feel worse. Call your PH nurse. Early intervention saves your heart.
Pulmonary hypertension isn’t a death sentence anymore. But it demands attention, expertise, and urgency. The tools are here. The knowledge is here. What’s missing is the awareness-on both sides of the exam room.
Can pulmonary hypertension be cured?
There is no cure for pulmonary hypertension yet, but modern therapies can significantly slow progression, improve symptoms, and extend life. Some patients with chronic thromboembolic PH (Group 4) may be cured with a surgical procedure called pulmonary thromboendarterectomy. For others, the goal is long-term management with combination drugs, lifestyle changes, and close monitoring. Sotatercept and other emerging therapies are showing potential to reverse artery damage, but they’re not widely available yet.
Is pulmonary hypertension the same as regular high blood pressure?
No. Regular high blood pressure (systemic hypertension) affects the arteries throughout your body. Pulmonary hypertension only affects the arteries between your heart and lungs. They’re measured differently, treated differently, and have different causes. You can have both at the same time, but one doesn’t cause the other. Treating systemic hypertension won’t fix PH.
How do I know if my right heart is strained?
Your doctor checks for right heart strain using echocardiography. Key signs include a thickened right ventricular wall (>5 mm), an enlarged right ventricle (area >22 cm²), and reduced TAPSE (<17 mm). Blood tests for BNP or NT-proBNP also rise when the right heart is under stress. If you’ve been diagnosed with PH, these should be checked every 3-6 months. If your TAPSE drops or your BNP rises, your treatment may need adjusting.
Can I still exercise with pulmonary hypertension?
Yes-but carefully. Exercise improves heart and lung function in PH patients, but overdoing it can be dangerous. Most specialists recommend supervised pulmonary rehabilitation programs. Walking, light cycling, and seated resistance training are safe for most. Avoid heavy lifting, holding your breath, or exercising in extreme heat or altitude. Always monitor your symptoms: if you feel dizzy, chest pain, or extreme shortness of breath, stop immediately and contact your care team.
Why do I need a right heart catheterization if my echo shows high pressure?
Echocardiograms estimate pressure-they don’t measure it directly. They can be off by 10-15 mmHg, leading to false positives or missed cases. Right heart catheterization gives exact numbers: mean pulmonary arterial pressure, pulmonary vascular resistance, and left heart pressures. This tells your doctor whether your PH is Group 1 (true PAH) or Group 2 (caused by left heart failure). The treatment is completely different. Without catheterization, you could get the wrong drugs-or miss a treatable cause like a blood clot.
What’s the life expectancy with pulmonary hypertension today?
In the 1980s, median survival after diagnosis was only 2.8 years. Today, with early diagnosis and combination therapy, 5-year survival rates are over 60%, according to the REVEAL Registry (2022). Some patients live 10, 15, or even 20 years with good quality of life. Survival depends on your group, how early you’re diagnosed, your response to treatment, and whether you’re under the care of a specialized PH center. The key is staying on therapy and monitoring your numbers closely.
What’s Next for Pulmonary Hypertension
The future is focused on earlier detection and targeting the root causes. The LIBERTY trial is testing let-7 microRNA as a blood marker that could flag right heart strain before symptoms appear. New drugs like dichloroacetate are being tested to improve how the right ventricle uses energy-something current drugs don’t touch.
But the biggest challenge isn’t science. It’s access. If you live in a rural area or lack insurance, getting diagnosed and treated on time is still a battle. That’s why patient advocacy and education matter. Knowing the signs, asking the right questions, and insisting on a referral to a PH center can make the difference between survival and decline.


Jay Powers
January 11, 2026 AT 21:10Been there. Thought I was just out of shape until I collapsed walking to my car. Doc said asthma. Turned out my pulmonary pressure was 42. No joke. They missed it for two years. Now I’m on triple therapy and actually breathing again. Don’t let anyone brush you off.
Alice Elanora Shepherd
January 12, 2026 AT 14:14Thank you for this incredibly detailed and compassionate overview. I particularly appreciate the emphasis on TAPSE and NT-proBNP thresholds-so many clinicians still rely solely on echo estimates. The 2022 diagnostic shift is critical, and yet, awareness remains shockingly low in primary care. I’ve seen patients wait over four years for diagnosis. Early detection is not just helpful-it’s lifesaving.
Christina Widodo
January 13, 2026 AT 19:26Wait so sotatercept actually reverses damage?? That’s wild. I thought PH was always progressive. Is this like a miracle drug or is it just for certain types? Also, is it even covered by insurance or is it like $500k a year??
Prachi Chauhan
January 15, 2026 AT 14:53life is a river and the heart is a boat. when the river gets narrow and rocky, the boat gets tired. it doesn’t mean the boat is broken. it means the river changed. we need to fix the river, not blame the boat. this is what ph is. not weakness. not aging. not anxiety. just a broken path. and we have tools now to fix it. but only if we look.
jordan shiyangeni
January 16, 2026 AT 07:43Let me be perfectly clear: this article is dangerously oversimplified. The notion that 'early diagnosis saves lives' ignores the fact that 70% of patients diagnosed with Group 1 PAH are misclassified due to inadequate catheterization protocols. The 2022 threshold change was a political move by the WHO, not a scientific one. And sotatercept? A glorified placebo with a $750,000 price tag. This is pharmaceutical theater masquerading as medicine. Real medicine is palliative care, not expensive, unproven cocktails that only benefit insurers and distributors.
Abner San Diego
January 17, 2026 AT 16:23U.S. has 35 centers? That’s pathetic. We got 300 million people and only 35 places that know how to treat this? Meanwhile, China’s got 120+ centers and they’re doing gene therapy trials. We’re falling behind because we let big pharma control everything. If this was cancer, we’d have a moonshot. But nope, it’s a lung thing-nobody cares.
Eileen Reilly
January 18, 2026 AT 15:43okay but like… i just googled TAPSE and now i think my dog has ph?? she gets tired after 2 minutes of chasing squirrels. also why is everyone so obsessed with numbers? my aunt had ph and she just drank green tea and danced. she lived 10 years longer than the docs said. maybe we just need less science and more vibes?
steve ker
January 20, 2026 AT 08:48Western medicine is a scam. In my village in Nigeria, we use bitter leaf and hot water. No catheters. No pumps. No $100k drugs. People live. You overcomplicate everything. Simplicity heals.
George Bridges
January 21, 2026 AT 14:57My sister was misdiagnosed for 3 years. She’s now on treprostinil and does yoga twice a week. She still gets tired, but she’s alive. I just want to say thank you for writing this without making people feel guilty. Awareness is the first step-and you’ve helped a lot of people take it.
gary ysturiz
January 22, 2026 AT 02:17YOU CAN DO THIS. I know it feels overwhelming. But every single person reading this has the power to ask one question: 'Could this be PH?' That one question could save your life-or someone you love. Don’t wait for perfection. Don’t wait for a specialist. Start the conversation. You’re not being dramatic. You’re being brave. And that matters.
Sumit Sharma
January 23, 2026 AT 03:44While the article is well-intentioned, it fails to address the fundamental flaw in PH management: the absence of standardized global diagnostic protocols. The reliance on echo alone is indefensible. Furthermore, the claim that combination therapy improves survival lacks robust longitudinal data beyond Phase II trials. Until we have Phase III RCTs across diverse populations, we are treating symptoms, not disease. This is not progress-it’s premature enthusiasm.
Darryl Perry
January 23, 2026 AT 09:57There is no such thing as 'right heart strain' in clinical practice. The term is misleading. The right ventricle hypertrophies or fails. There is no in-between. The author is using emotionally manipulative language to create false urgency. This is not medicine. This is marketing.
Windie Wilson
January 23, 2026 AT 20:00So let me get this straight… we have a disease that kills people slowly, doctors ignore it for years, and the solution is… more drugs? More machines? More $$$? 😂 I’m just here waiting for the TikTok trend: #PHSurvivorDanceChallenge with IV pumps and oxygen tanks. Because nothing says ‘hope’ like a 6-minute walk test set to pop music.
Monica Puglia
January 24, 2026 AT 22:13My mom’s on epoprostenol and she’s been doing great 🥹 But the pump beeps at 3am and I have to change the tubing… it’s a lot. But I’d do it 1000 times. This post made me cry. Not because it’s sad-because it’s true. We’re not alone. 💙