Why Medication Labels Matter More Than You Think
Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these mistakes happen not because someone took the wrong pill, but because they didn’t understand what the label actually said. A parent gives their child too much cough syrup because they used a kitchen spoon. An older adult doubles up on painkillers because they missed the warning about acetaminophen. Someone takes an entire bottle of liquid antibiotic thinking it’s one dose. These aren’t rare accidents-they’re predictable results of unclear labels and rushed reading.
Medication labels aren’t just legal paperwork. They’re your safety manual. Whether it’s a prescription from your doctor or a bottle of ibuprofen from the shelf, the label tells you exactly how to use the medicine safely-and what happens if you don’t. The FDA made these labels standard for a reason: to cut down on confusion, prevent overdoses, and stop dangerous interactions before they start.
What’s on a Prescription Label (And What You Can’t Ignore)
Prescription labels follow strict federal rules. They’re designed to give your pharmacist and doctor all the details they need-and for you, the most critical ones. Here’s what you’ll find on every prescription bottle:
- Your name - Always check this first. Mixing up names is one of the most common pharmacy errors.
- Medicine name - Both the brand name (like Lipitor) and the generic (atorvastatin). If you’re unsure, ask your pharmacist to confirm.
- Dosage and instructions - This is the most important part. It tells you how much to take and how often. Look for phrases like “take one tablet by mouth twice daily” or “10 mL every 6 hours as needed.” Don’t assume “twice daily” means morning and night-it could mean every 12 hours. Ask if you’re not sure.
- Expiration date - Most pharmacies set this for one year after dispensing, even if the bottle says it lasts longer. Expired meds can lose strength or become unsafe.
- Pharmacy info - Name, phone number, address. Keep this handy in case you have questions.
- Warnings - These are bold for a reason. Things like “May cause drowsiness,” “Avoid alcohol,” or “Take on an empty stomach” aren’t suggestions-they’re safety rules.
For serious drugs-like blood thinners, insulin, or chemotherapy-there’s often a separate Medication Guide. These are printed handouts you should read carefully. The FDA requires them for 153 high-risk medications, including HIV drugs and isotretinoin. Don’t just take the bottle. Ask for the guide.
Decoding OTC Labels: The Drug Facts Box
Over-the-counter (OTC) meds like Tylenol, Benadryl, or Cold & Flu tablets have to follow the FDA’s “Drug Facts” format. It’s the same layout on every bottle, so once you learn it, you can read any OTC label quickly.
Here’s how it breaks down:
- Active Ingredient(s) - This lists the medicine’s key chemical. For example, “Acetaminophen 325 mg.” This is the part that actually treats your symptoms. Many cold and flu products contain the same active ingredient. Taking more than one can lead to overdose.
- Purpose - What the ingredient does. “Pain reliever,” “cough suppressant,” “antihistamine.”
- Uses - Symptoms it treats. “Relieves headache, fever, sore throat.”
- Warnings - This section is where most people skip. It tells you who shouldn’t take it, what to avoid (like alcohol or other meds), and signs of trouble. For example: “Do not use if you have liver disease” or “May cause drowsiness.”
- Directions - How much to take, how often, and for how long. “Adults: Take 1 tablet every 4 to 6 hours. Do not exceed 4 tablets in 24 hours.” Never go over this limit, even if you feel worse.
- Inactive Ingredients - Fillers, dyes, flavors. Important if you have allergies. For example, some people react to dyes like FD&C Red No. 40.
- Other Information - Storage tips, like “Keep at room temperature.”
One big red flag: if a product says “multi-symptom,” it likely contains multiple active ingredients. Taking it with another cold medicine could mean you’re doubling up on acetaminophen or pseudoephedrine-both of which can be dangerous in high doses.
How to Read Liquid Medication Labels (And Avoid Deadly Mistakes)
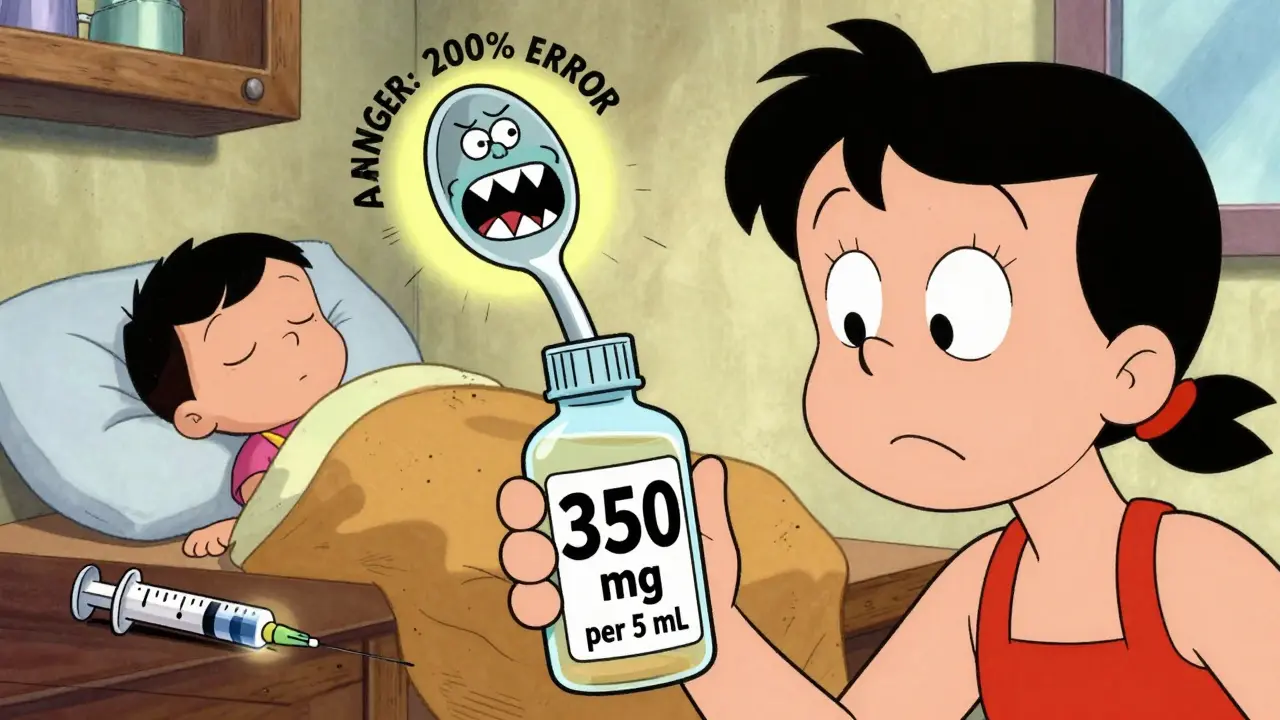
Liquid medicines are the most dangerous when misread. Why? Because dosing depends on concentration-and most people don’t know how to calculate it.
Look for this line: “350 mg per 5 mL.” That means every 5 milliliters contains 350 mg of medicine. If your doctor orders 700 mg, you need to give 10 mL-not 700 drops, not two teaspoons, not “a capful.”
Here’s how to get it right:
- Find the concentration: “X mg per Y mL.”
- Divide the total dose by the concentration to find how many mL you need.
- Use only the measuring tool that came with the bottle-usually an oral syringe or dosing cup.
Never use a kitchen spoon. A teaspoon from your drawer can hold anywhere from 2.5 mL to 7.3 mL. That’s a 200% difference. In children, that’s the difference between a safe dose and a toxic one.
Parents of young kids are especially at risk. A 2022 study found 68% of caregivers made errors when measuring liquid meds for their children. The fix? Buy a $3 oral syringe from the pharmacy. Write the dose on it with a marker. Store it with the medicine.
What to Do When the Label Doesn’t Make Sense
Confused by “take on an empty stomach”? Not sure if “every 8 hours” means 6 a.m., 2 p.m., 10 p.m.? Wondering if you can crush a pill or open a capsule?
Don’t guess. Don’t ask a friend. Don’t search Google and hope for the best.
Call your pharmacist. They’re trained to explain labels in plain language. They can tell you:
- Whether you can split a tablet
- If a medicine interacts with your other prescriptions
- How to store it properly
- What side effects are normal vs. dangerous
Pharmacists are your best line of defense. In fact, the American Nurses Association says the “Five Rights” of safe medication use-right patient, right drug, right dose, right route, right time-all start with reading the label correctly. And if you’re still unsure, ask for a written copy of the instructions. Most pharmacies will print them for you.
Common Mistakes That Lead to Hospital Visits
Emergency rooms see hundreds of cases every month from medication errors. Here are the top three reasons:
- Doubling up on the same ingredient - Taking Tylenol and a cold medicine that also has acetaminophen. That’s how people end up with liver failure.
- Ignoring expiration dates - Old insulin, antibiotics, or epinephrine pens can fail when you need them most.
- Not reading the warnings - Taking a sleep aid with alcohol, or a painkiller with blood pressure meds. These interactions can be deadly.
One study found that 53% of patients never read the “dosage modifications” section-like what to do if you have kidney disease or are over 65. If you have chronic conditions, this part is critical. Your dose might need to be lower.
And here’s something surprising: 31% of people admit they don’t even read the label. That’s not laziness-it’s overwhelm. But the fix is simple: slow down. Take the bottle to a quiet place. Read it out loud. Ask someone else to read it with you.
What’s Changing: Safer Labels for the Future
The FDA and health groups are working to make labels easier to understand. By 2024, more prescriptions will include QR codes that link to video instructions. Some new labels already use icons for warnings-like a skull for toxicity or a clock for timing.
Plain language is now required for high-alert drugs like insulin and opioids. Instead of “Administer subcutaneously,” you’ll see “Inject under the skin.”
By 2027, global standards will likely include color-coded labels: red for high-risk drugs, yellow for caution, green for routine. This is already being tested in hospitals.
But until then, you’re still the most important safety check. No matter how good the label gets, you still have to read it.
Quick Checklist: Before You Take Any Medicine
- ✔️ Is this medicine for me? (Check name)
- ✔️ Is this the right drug? (Compare name to prescription)
- ✔️ Do I know the dosage? (How many mg/mL? How often?)
- ✔️ Am I using the right tool? (Syringe, not spoon)
- ✔️ Did I check for duplicate ingredients? (Especially in OTC combos)
- ✔️ Did I read the warnings? (Allergies, alcohol, driving, etc.)
- ✔️ Is it expired? (Check date)
- ✔️ Do I have questions? (Call your pharmacist)
Frequently Asked Questions
What should I do if my medication label looks different from last time?
Always check with your pharmacist. Even small changes-like a different color, shape, or wording-could mean a new generic version, a different strength, or a reformulated product. Don’t assume it’s the same. Confirm the active ingredient and dosage match your prescription.
Can I trust the dosage instructions on the bottle if my doctor told me something different?
Your doctor’s instructions override the label. But if there’s a mismatch, call your doctor’s office or pharmacist immediately. It could be a labeling error, a typo, or a special adjustment. Never take a dose that contradicts your doctor’s orders without confirming it first.
Why do some medicine labels say “take with food” and others say “take on an empty stomach”?
Some medicines work better or cause fewer side effects depending on whether your stomach is full or empty. For example, antibiotics like tetracycline can’t be absorbed well with dairy, while others like ibuprofen can irritate your stomach if taken on an empty stomach. The label tells you what’s safest and most effective for that specific drug.
Is it safe to crush pills or open capsules?
Only if the label or your pharmacist says it’s okay. Many pills are designed to release slowly over time. Crushing them can cause too much medicine to enter your body at once. Some capsules contain powders that are dangerous to inhale. Always ask before altering the form.
What if I miss a dose? Should I double up next time?
Never double up unless the label says so. For most medicines, if you miss a dose, take it as soon as you remember-but if it’s almost time for the next one, skip the missed dose. Taking too much can be dangerous. Check the label’s “missed dose” section or call your pharmacist for advice.


Solomon Ahonsi
February 1, 2026 AT 21:22George Firican
February 3, 2026 AT 17:36Matt W
February 3, 2026 AT 19:13Anthony Massirman
February 5, 2026 AT 07:49Eli Kiseop
February 6, 2026 AT 02:16Akhona Myeki
February 7, 2026 AT 02:02Brittany Marioni
February 7, 2026 AT 06:51Murarikar Satishwar
February 7, 2026 AT 08:24larry keenan
February 7, 2026 AT 21:24Chinmoy Kumar
February 9, 2026 AT 20:45Brett MacDonald
February 10, 2026 AT 13:33Sandeep Kumar
February 10, 2026 AT 22:06Gary Mitts
February 11, 2026 AT 04:06