Why NTI Drugs Are Different
Not all generic drugs are created equal. For most medications, switching from brand to generic causes no issues. But for NTI drugs-narrow therapeutic index drugs-even tiny changes in dosage can lead to serious harm. These are drugs where the difference between a safe dose and a toxic one is razor-thin. Think warfarin, lithium, levothyroxine, phenytoin, and digoxin. A 5% change in blood levels might mean the difference between control and crisis. For someone on warfarin, a slightly stronger generic could cause a dangerous bleed. For someone with epilepsy, a weaker version could trigger a seizure.
The FDA says these drugs don’t need special rules. Since 1997, they’ve maintained that the same 80-125% bioequivalence range used for all generics is fine-even for NTI drugs. But doctors and pharmacists who work with these patients every day know better. Studies show that 32.4% of patients stabilized on brand-name levothyroxine see their thyroid hormone levels shift after switching to a generic. That’s not a small number. It’s enough to require dose adjustments, extra blood tests, and sometimes hospital visits.
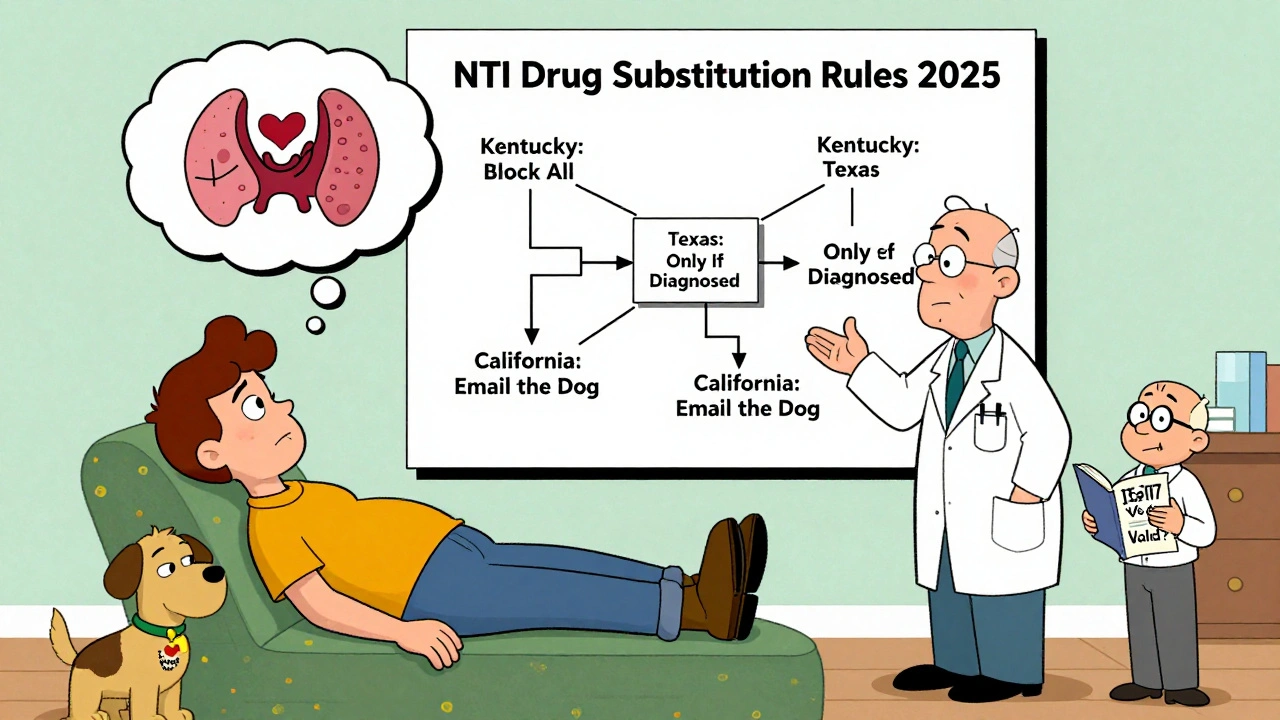
States Are Taking Matters Into Their Own Hands
While the FDA holds its line, 27 states have passed laws that restrict or ban generic substitution for NTI drugs. These aren’t suggestions. These are legal requirements. And they’re wildly different from state to state.
In Kentucky, pharmacists can’t substitute any drug on their official NTI list-no exceptions. That list includes digitalis, antiepileptics, and warfarin. If a prescription says Synthroid, you get Synthroid. If it says Coumadin, you get Coumadin. Same in Pennsylvania. They have their own list, and it’s enforceable by law. Violate it, and you risk losing your license.
South Carolina doesn’t ban substitutions outright. Instead, they recommend against it for three categories: NTI drugs like lithium, specific brand-name drugs like Premarin and Synthroid, and what they call “critical drugs”-including insulin, anticoagulants, and time-release asthma meds. Pharmacists can still substitute, but they’re expected to know the risks and document their reasoning. It’s a gray zone, and pharmacists have to be extra careful.
Tennessee takes a middle path. They allow substitution of A-rated generics, unless the drug is an antiepileptic used for epilepsy or seizures. Then, no substitution-period. This is a targeted rule, not a blanket ban. It shows how states are learning to be more precise instead of sweeping everything under one label.
California and Texas: Two Very Different Models
California doesn’t have a list of NTI drugs. Instead, they define the problem by effect. Their law says any drug where a 10% or less change in blood concentration could be dangerous counts as a “critical dose drug.” That includes warfarin, levothyroxine, and phenytoin, but also some newer drugs the FDA hasn’t flagged. When a pharmacist substitutes one of these, they must notify the prescriber in writing. It’s not a ban-it’s a transparency rule. The goal is to keep everyone in the loop.
Texas goes even narrower. Their law only prohibits substitution of anticonvulsants for patients with epilepsy. No mention of warfarin. No mention of lithium. Just one specific patient group. This means a person with bipolar disorder taking carbamazepine might be allowed to switch generics, but someone with epilepsy taking the same drug can’t. It’s a legal distinction based on diagnosis, not drug class.

The Real Cost of Confusion
Imagine you’re a pharmacist working for a chain that spans five states. One day you’re filling a prescription in Nashville. You know Tennessee’s rule: no substitution for antiepileptics in epilepsy patients. The next day you’re in Chattanooga, same state, same pharmacy system-but the regional manager says, “We’ve had complaints, so we’re being extra cautious. Don’t substitute even if the patient doesn’t have epilepsy.” Now you’re confused. Which rule do you follow? The law? The policy? The unwritten office rule?
A 2023 survey found that 68.3% of pharmacists working across state lines have been confused about NTI substitution rules. Over 40% admitted they accidentally broke a law in the past year. That’s not negligence. That’s a system that’s broken.
Pharmacy benefit managers like Express Scripts say NTI substitution rules have increased their administrative costs by 5.7%. Why? Because they have to build custom rules into their software for each state. Prescribers have to fill out extra forms. Pharmacies have to train staff on five different sets of rules. Patients get inconsistent care. And the worst part? Many don’t even know they’ve been switched.
What’s Changing in 2025
Pressure is building to fix this mess. In January 2024, the National Association of Boards of Pharmacy released a Model State NTI Substitution Act. It’s a standardized list of NTI drugs based on clinical evidence-not state politics. Twelve states have already introduced it as legislation. That’s a big deal.
And the FDA? They’re finally listening. In September 2024, they announced they’d reconsider their 27-year-old stance after the Senate Committee on Aging cited a Government Accountability Office report showing nearly 3,000 adverse events linked to NTI drug substitutions between 2019 and 2023. That’s not a glitch. That’s a pattern.
Even the Department of Labor weighed in. Their January 2025 opinion letter said that if a patient needs strict NTI drug control to stay healthy, that could affect their eligibility for medical leave under FMLA. It’s a quiet signal: this isn’t just a pharmacy issue. It’s a public health issue.
What This Means for Patients
If you’re on warfarin, levothyroxine, or any drug with a narrow therapeutic index, here’s what you need to do:
- Ask your pharmacist: “Is this the same brand I’ve been taking?”
- Check your prescription bottle. If the name changed, ask why.
- Know your state’s rules. Some states require you to sign a form if you want to switch. Others require the doctor to write “dispense as written.”
- Monitor your symptoms. If you feel different after a refill-fatigue, dizziness, irregular heartbeat, mood swings-call your doctor. Don’t wait.
Don’t assume generics are always interchangeable. For NTI drugs, they’re not. Your safety depends on knowing the rules-and speaking up.
What’s Next for NTI Drug Rules
By 2027, experts predict 38 states will have adopted standardized NTI substitution rules. That’s up from 27 today. The goal? Fewer errors, less confusion, and better outcomes. But it won’t be easy. Drug companies, pharmacy chains, and insurers all have financial stakes in keeping substitution easy. The fight isn’t over.
For now, the system is a patchwork. And the only person who can protect you in that mess is you.
What exactly is an NTI drug?
An NTI drug, or narrow therapeutic index drug, is a medication where small changes in dosage or blood concentration can cause serious side effects or treatment failure. Examples include warfarin (blood thinner), levothyroxine (thyroid hormone), lithium (mood stabilizer), and phenytoin (anti-seizure). The difference between a safe level and a toxic one is very small-sometimes less than 10%.
Can I be switched to a generic NTI drug without my knowledge?
In many states, yes-unless your doctor writes "dispense as written" on the prescription. Some states require pharmacists to notify you or your doctor before switching. Others don’t. Always check your prescription label. If the drug name or manufacturer changed, ask why.
Which states ban NTI drug substitution completely?
Kentucky and Pennsylvania have formal lists of NTI drugs that cannot be substituted under any circumstances. Other states like South Carolina and California don’t ban substitution outright but require extra steps-like notifying the prescriber or avoiding substitution for certain patient groups.
Why does the FDA allow substitution if it’s risky?
The FDA says the current bioequivalence standards (80-125% blood concentration range) are safe for all drugs, including NTI drugs. They argue that generic manufacturers meet the same quality standards. But critics point out that even within that range, small shifts can harm sensitive patients-especially those on levothyroxine or warfarin. The FDA has acknowledged this debate and is reviewing its position as of late 2024.
What should I do if I think a substitution caused a problem?
Contact your doctor immediately. If you’ve had new symptoms like fatigue, heart palpitations, mood changes, or seizures after a refill, it could be related to a drug switch. Request your blood test results before and after the change. Report the incident to your state board of pharmacy. And always ask for the same brand next time-write "dispense as written" on future prescriptions.


Hamza Laassili
December 14, 2025 AT 04:50Sheldon Bird
December 14, 2025 AT 16:24Lauren Scrima
December 15, 2025 AT 16:06Jennifer Taylor
December 16, 2025 AT 21:16Cole Newman
December 18, 2025 AT 20:45nina nakamura
December 20, 2025 AT 15:51Ronan Lansbury
December 22, 2025 AT 15:00Emma Sbarge
December 22, 2025 AT 22:50Constantine Vigderman
December 23, 2025 AT 06:19Harriet Wollaston
December 25, 2025 AT 03:21Karen Mccullouch
December 27, 2025 AT 02:15sharon soila
December 27, 2025 AT 13:41Michael Gardner
December 27, 2025 AT 15:36