Beta-Blocker Selection Tool
Select your primary condition and any relevant health factors to see which beta-blocker types might be most appropriate for you.
Not all beta-blockers are the same. Even though they all work by blocking adrenaline, the differences between them can mean the difference between feeling better and feeling worse. If you’ve been prescribed one and are wondering why your doctor chose it over another, or if you’ve noticed side effects others didn’t, the answer isn’t just about your heart-it’s about which receptors the drug hits, how it’s made, and what else it does beyond slowing your pulse.
What Beta-Blockers Actually Do
Beta-blockers stop adrenaline and noradrenaline from binding to beta receptors in your heart and blood vessels. This reduces your heart rate, lowers blood pressure, and decreases the force of each heartbeat. Less work for your heart means less oxygen needed-which is why they’re used after heart attacks, for angina, and in heart failure. But they don’t just act on the heart. Some also affect your lungs, blood vessels, and even your brain.
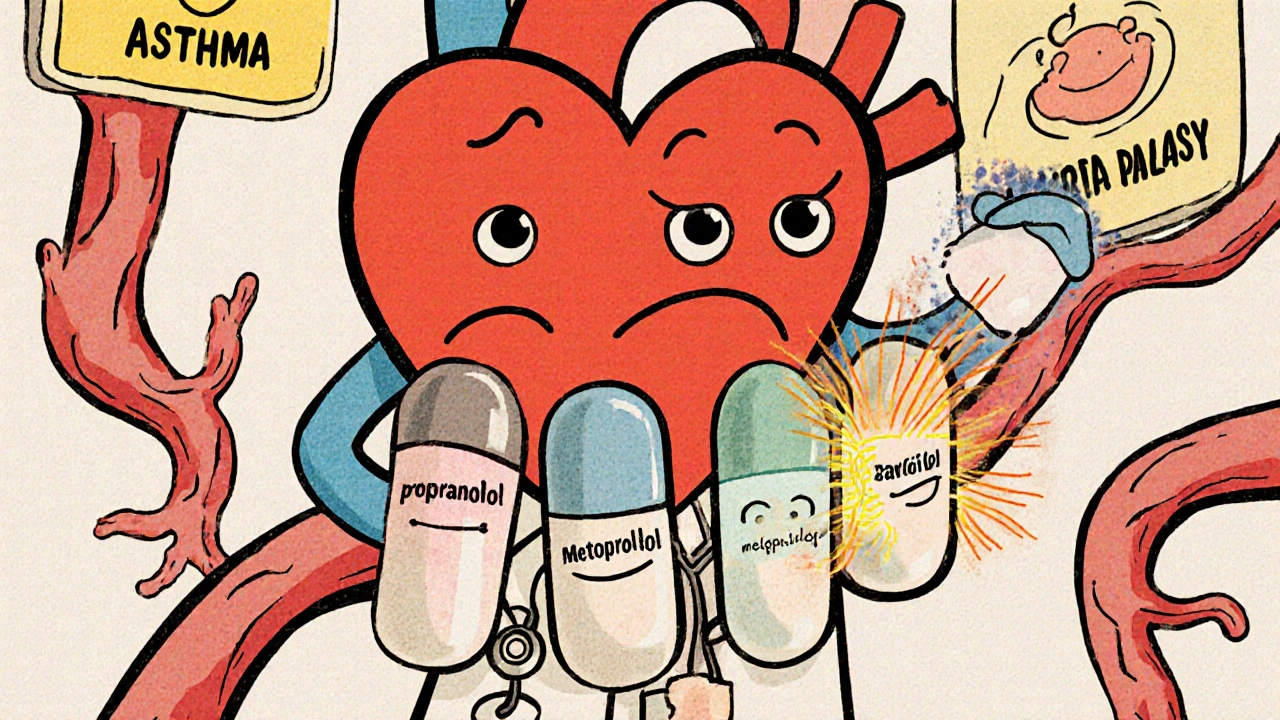
The first beta-blocker, propranolol, came out in the 1960s. It was a game-changer for heart patients. Today, we have more than 15 types, grouped into three generations based on how specific they are and what extra effects they have. Knowing which generation you’re on helps explain why one drug works for you and another doesn’t.
First-Generation: Non-Selective and Broad Effects
Propranolol, labetalol, and sotalol belong here. They block both beta-1 (heart) and beta-2 (lungs, blood vessels, liver) receptors. That means they slow your heart-but they can also tighten your airways. If you have asthma or COPD, this can be dangerous. A 2022 study in the Journal of the American College of Cardiology found that patients on non-selective beta-blockers had a 20-30% higher risk of bronchospasm compared to those on selective ones.
Propranolol also crosses the blood-brain barrier. That’s why some people on it report nightmares, depression, or fatigue. In patient reviews on Drugs.com, 38% said they had moderate to severe side effects, with sleep problems and exercise intolerance being common. It’s still used-for migraines, tremors, and anxiety-but not as a first choice for heart conditions anymore, especially when better options exist.
Second-Generation: Heart-Selective and Safer for Lungs
Atenolol, metoprolol, and bisoprolol are the big names here. These drugs mainly target beta-1 receptors, so they’re gentler on your lungs. That’s why they’re preferred for people with mild asthma or COPD-even though doctors still monitor them closely.
Metoprolol comes in two forms: tartrate (short-acting, taken twice daily) and succinate (long-acting, once daily). The succinate version is better for heart failure because it keeps levels steady. A 2022 Cleveland Clinic survey found 85% of heart failure patients stuck with metoprolol succinate because it caused fewer breathing issues than propranolol.
Bisoprolol is another favorite. It’s clean, predictable, and rarely causes fatigue. Patient ratings on Drugs.com give it a 7.1/10, while propranolol sits at 6.2/10. That gap isn’t just luck-it’s pharmacology. Bisoprolol is mostly cleared by the kidneys, so it’s easier to dose in older adults. Metoprolol is broken down by the liver, so it can build up if you have liver problems.
Third-Generation: The Game Changers
Carvedilol and nebivolol aren’t just beta-blockers-they’re multitaskers.
Carvedilol blocks beta-1 and beta-2 receptors, but also blocks alpha-1 receptors. That means it doesn’t just slow your heart-it opens up your blood vessels. In the US Carvedilol Heart Failure Study (1996), it cut death risk by 35% compared to placebo. That’s why the European Society of Cardiology now lists it as a top choice for heart failure with reduced ejection fraction. It also reduces oxidative stress in heart tissue by 30-40% in lab studies, which helps prevent scarring.
Nebivolol is even more unique. It activates beta-3 receptors, which triggers your body to make more nitric oxide. That’s the same molecule that makes Viagra work-so it helps blood vessels relax and improves circulation. In the SENIORS trial, it lowered cardiovascular death by 14% in elderly heart failure patients. And because it doesn’t lower testosterone or reduce blood flow to the genitals, men on nebivolol report better sexual function than those on older beta-blockers. A Reddit thread from a cardiac nurse in 2023 noted that 65% of male patients over 50 saw improvement in erectile function after switching to nebivolol.
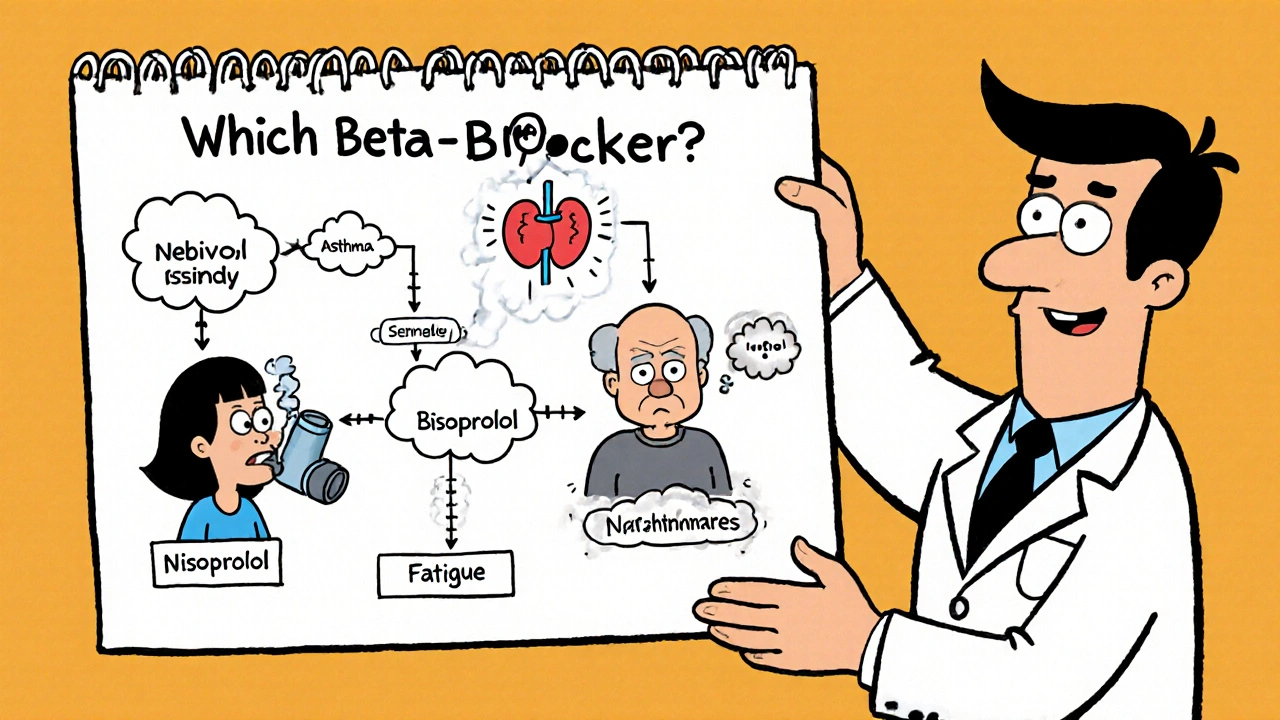
Why One Drug Works for You-and Not Someone Else
Two people with the same diagnosis might get completely different beta-blockers. Why?
- Heart failure? Carvedilol or nebivolol are first-line. They improve survival. Metoprolol succinate is also approved, but tartrate isn’t.
- High blood pressure? Beta-blockers aren’t first choice anymore. The 2023 Mayo Clinic guidelines say ACE inhibitors or calcium channel blockers lower central aortic pressure better. But if you’ve had a heart attack, you still need one-carvedilol or bisoprolol are preferred.
- Asthma or COPD? Avoid propranolol. Use bisoprolol or nebivolol instead. Even then, start low and go slow.
- Depression or fatigue? Propranolol is the worst offender. Switch to bisoprolol or nebivolol-both have lower rates of mood side effects.
- Elderly patient? Avoid high doses. Use lower starting doses. Nebivolol and bisoprolol are easier to titrate safely.
Also, timing matters. Carvedilol must be titrated slowly-starting at 3.125 mg twice daily, increasing every 2 weeks over 8-16 weeks. Rush it, and you risk low blood pressure and dizziness. Bisoprolol can be ramped up in 4-8 weeks. Metoprolol succinate is once daily; metoprolol tartrate is not. Mixing them up can lead to under- or overdosing.
What Happens If You Stop Suddenly?
Never quit beta-blockers cold turkey. The FDA issued a warning in 2021: stopping abruptly can spike your heart rate and blood pressure, increasing your risk of heart attack by 300% in the first 48 hours. This is true for all types-even if you’ve only been on it for a few weeks. Always taper down over 1-2 weeks under medical supervision.
Drug Interactions to Watch For
Beta-blockers don’t play well with everything.
- Calcium channel blockers (verapamil, diltiazem): Can cause dangerously slow heart rates when combined with beta-blockers.
- Insulin or diabetes meds: Beta-blockers can mask low blood sugar symptoms like shaking and fast heartbeat. You might not know you’re hypoglycemic until it’s serious.
- Albuterol inhalers: Non-selective beta-blockers like propranolol can block the effect of these rescue inhalers by up to 50%. If you’re on one, your asthma control could collapse during an attack.
- SSRIs (like fluoxetine): Can slow how your liver breaks down metoprolol, leading to higher levels and more side effects.
What’s New in 2025?
The field is evolving. In 2023, the FDA approved entricarone-a new drug that blocks beta-1 receptors while activating beta-3 receptors, designed for heart failure with preserved ejection fraction. Early results show a 22% drop in hospitalizations.
Also coming: a combo pill of nebivolol and valsartan (an ARB), expected in 2024. It’s meant to simplify treatment for patients needing both blood pressure control and heart protection.
Researchers are even testing gene-based selection. The GENETIC-BB trial is looking at whether your DNA can predict which beta-blocker you’ll respond to best-based on how your body metabolizes them or how your receptors are built. It’s early, but it could one day mean no more trial-and-error.
Bottom Line: It’s Not One-Size-Fits-All
Beta-blockers are powerful-but they’re not interchangeable. Propranolol isn’t better than nebivolol. Bisoprolol isn’t weaker than carvedilol. Each has a role. Your doctor doesn’t just pick a name-they pick a mechanism, a side effect profile, a dosing schedule, and a safety net for your other conditions.
If you’re on a beta-blocker and feel off-fatigued, cold, depressed, or short of breath-don’t assume it’s just part of the deal. Ask: Could this be the drug? Is there a better fit? Your heart isn’t the only thing that matters.
Are beta-blockers still used for high blood pressure?
Yes-but not as a first choice for simple high blood pressure without other heart conditions. Guidelines from Mayo Clinic (2023) and the American Heart Association now prefer ACE inhibitors, ARBs, or calcium channel blockers because they lower central aortic pressure more effectively. Beta-blockers are still used if you’ve had a heart attack, have heart failure, arrhythmias, or migraines. They’re not outdated-they’re specialized.
Which beta-blocker has the least side effects?
Bisoprolol and nebivolol tend to have the lowest rates of fatigue, depression, and cold extremities based on patient surveys and clinical data. Bisoprolol is clean, predictable, and rarely causes sleep issues. Nebivolol adds the benefit of better circulation and fewer sexual side effects in men. Propranolol has the highest side effect burden, especially on mood and energy.
Can I take a beta-blocker if I have asthma?
It’s risky with non-selective ones like propranolol-they can trigger severe bronchospasm. But cardioselective beta-blockers like bisoprolol, metoprolol succinate, or nebivolol are often tolerated at low doses, especially if your asthma is mild and well-controlled. Your doctor will start you on the lowest possible dose and monitor you closely. Never take a non-selective beta-blocker if you have active asthma.
Why does carvedilol help heart failure more than older beta-blockers?
Carvedilol doesn’t just slow the heart-it also opens blood vessels by blocking alpha-1 receptors. This reduces strain on the heart and improves blood flow. It also reduces oxidative stress in heart muscle by 30-40%, which helps prevent scarring and remodeling. In clinical trials, it cut death rates by 35% compared to placebo. No older beta-blocker has shown that level of benefit.
Do beta-blockers cause weight gain?
Some do, especially older ones like propranolol and atenolol. They can slow metabolism slightly and reduce physical activity due to fatigue. Nebivolol and carvedilol are less likely to cause weight gain. If you notice unexplained weight gain after starting a beta-blocker, talk to your doctor-it might be fluid retention or reduced activity, not fat.
How long does it take for beta-blockers to work?
For heart rate and blood pressure, you’ll usually see effects within a few hours to a day. But for heart failure or post-heart attack benefits, it takes weeks to months. The full protective effect-like reducing scar tissue or improving survival-can take 3-6 months. That’s why doctors don’t judge effectiveness after just two weeks.
Can I exercise while on beta-blockers?
Yes-but you’ll feel different. Your heart won’t race as much during exercise, so your perceived effort might feel higher than it is. Don’t rely on heart rate to gauge intensity. Use the "talk test"-if you can speak in short sentences but not sing, you’re in the right zone. Beta-blockers protect your heart during activity, so exercise is encouraged, just adjust how you measure it.

Alexa Ara
October 30, 2025 AT 23:25Just wanted to say this post saved my life. I was on propranolol for anxiety and felt like a zombie-no energy, nightmares every night. Switched to bisoprolol after reading this and now I can actually jog again. Thank you for explaining the differences so clearly.
Doctors never tell you how much the drug itself can change your whole life. This isn’t just medicine-it’s quality of life.
Also, nebivolol for the win. My husband switched and says he finally feels like himself again. No more ED issues. Huge relief.
Don’t suffer in silence. Ask your doc if there’s a better fit. You deserve to feel good, not just alive.
Love this kind of deep dive. More like this please!
Olan Kinsella
October 31, 2025 AT 03:37you ever wonder if beta-blockers are just the pharmaceutical industry’s way of making you forget you’re alive? we’ve turned human experience into a chemical equation. your heartbeat? a number. your sadness? a receptor imbalance. your joy? an unmeasured variable.
propranolol doesn’t fix anxiety-it silences the scream. and we call that treatment?
the real question: are we healing people… or just training them to be quieter?
also, the FDA warning about abrupt discontinuation? that’s not safety-that’s dependency engineering. ask yourself why they don’t warn you about the cost of emotional numbness.
we’re not treating hearts. we’re managing symptoms of a broken system.
Kat Sal
October 31, 2025 AT 06:49Okay but can we talk about how amazing it is that we’ve moved from ‘one-size-fits-all’ propranolol to drugs that actually respect your body’s uniqueness?
It’s like going from a blunt hammer to a precision scalpel. Nebivolol helping with circulation? Carvedilol reducing scarring? That’s not just science-that’s hope.
And the fact that we’re now looking at genetic matching? That’s the future. Imagine a world where your DNA tells your doctor exactly what you need. No more guessing. No more side effects.
I’m not a doctor but I’ve been on three different beta-blockers. This post nailed it. You’re not broken-you’re just waiting for the right match.
Also, never stop cold turkey. I did once. Felt like my heart was trying to escape my chest. Never again.
Rebecca Breslin
October 31, 2025 AT 21:36Okay I’ve got to correct something. You said bisoprolol is cleared by the kidneys-that’s correct-but you missed that it’s also one of the few beta-blockers with zero active metabolites. That’s why it’s so clean. Metoprolol? It’s got five metabolites, some of which are still pharmacologically active. That’s why people get weird side effects even when their dose seems ‘right.’
Also, the 2023 Mayo Clinic guidelines? They specifically say beta-blockers are second-line for hypertension ONLY if there’s no comorbidity. But if you’ve had a myocardial infarction? First-line, no debate.
And carvedilol’s 35% mortality reduction? That’s from the COMET trial, not the US Carvedilol HF Study. The US one was 6.5%. Big difference.
Also, nebivolol’s nitric oxide effect? It’s dose-dependent. At 5mg it’s minimal. At 10mg it’s significant. Most docs start at 2.5mg and wonder why it ‘doesn’t work.’
And yes, propranolol causes weight gain. But it’s not metabolism-it’s fluid retention from reduced cardiac output. Nebivolol doesn’t do that. Because it vasodilates. That’s why it’s better for obese patients.
Also, SSRIs slowing metoprolol metabolism? That’s CYP2D6. Fluoxetine is a strong inhibitor. Paroxetine too. Sertraline? Mild. Escitalopram? Negligible. Know your SSRI.
And if you’re on verapamil + beta-blocker? You need a pacemaker. No joke. I’ve seen three cardiac arrests from that combo.
Kierstead January
November 2, 2025 AT 16:18Let’s be real-beta-blockers are just a Band-Aid for people who won’t fix their lives.
You’re stressed? Don’t take a pill. Quit your toxic job. Stop scrolling. Get sunlight. Move your body. Sleep. Eat real food.
Instead, we give you a drug that makes you numb so you can keep living the same miserable life.
And now we’ve got ‘genetic matching’? That’s not progress-that’s corporate greed in a lab coat. You think your DNA is the problem? No. Your lifestyle is.
And nebivolol helps with erectile function? Wow. So we’re now selling heart meds as performance enhancers? Great. Next up: antidepressants for better TikTok engagement.
Stop outsourcing your well-being to Big Pharma. Your body isn’t a machine you can tweak with a pill. It’s a temple. And you’re treating it like a car you can just swap parts in.
Also, if you’re on beta-blockers and can’t exercise? Maybe you don’t need them. Maybe you need a therapist.
Just saying.
Imogen Levermore
November 4, 2025 AT 16:11okay but what if beta blockers are part of a secret mind control program? 🤔
i mean think about it-why do they make you feel ‘calm’? why do they reduce your heart rate so perfectly? why do they disappear from your system so neatly? 🤔
and why do they never mention the 1970s CIA experiments with propranolol? 🤔
also the FDA warning? that’s a cover-up. they don’t want you to know how addictive they are. it’s not withdrawal-it’s soul extraction. 💀
and nebivolol helping with erections? that’s not science. that’s a backdoor to the patriarchy. 🤫
and gene testing? they’re mapping your DNA so they can predict your rebellion levels. you think they want you to feel good? no. they want you to be predictable.
just sayin’… i’m off the meds. i’m going to meditate under a tree. 🌳✨
also the ‘2025 entricarone’? that’s a code name for Project Bluebird. i’ve seen the documents. 🕵️♀️
Chris Dockter
November 5, 2025 AT 01:30Propranolol is the worst drug ever made and doctors are lazy for prescribing it
My cousin died from a bronchospasm on propranolol for migraines
They didn't even test for asthma first
Just gave him the script
Now he's gone
And everyone acts like it's normal
It's not
Stop prescribing the old stuff
Bisoprolol or nebivolol
That's it
End of story
Don't let your doctor gamble with your life
Ask for the right one
Or find a new doctor
Gordon Oluoch
November 6, 2025 AT 12:06Let’s address the elephant in the room: most patients don’t understand what they’re taking and doctors don’t have time to explain it. That’s not negligence-it’s systemic failure.
You’re handed a prescription like a candy bar and expected to trust it. But beta-blockers aren’t candy. They alter your physiology at a molecular level. You’re not just slowing your heart-you’re changing your neurochemistry, your vascular tone, your metabolic response.
And yet, patients are expected to self-manage complex dosing schedules, drug interactions, and side effects with zero education.
The fact that people are switching from propranolol to nebivolol because of sexual dysfunction? That’s not a win. That’s a tragedy. We’ve reduced human experience to side effect profiles.
And the genetic trials? They’re not about precision medicine. They’re about patent extension. The industry needs new revenue streams. You’re not a patient-you’re a data point.
Don’t get me wrong-these drugs save lives. But the system that delivers them? It’s broken.
And if you’re taking one because your doctor didn’t have time to talk? You’re not being treated. You’re being managed.
That’s not healthcare. That’s triage with a prescription pad.
Tyler Wolfe
November 8, 2025 AT 04:32I’m a nurse and I’ve seen this play out a thousand times. Someone comes in with high BP and gets propranolol because it’s cheap. Then they come back six months later saying they can’t sleep, can’t exercise, and feel like they’re underwater.
We switch them to bisoprolol and they cry because they feel like themselves again.
It’s not magic. It’s pharmacology.
Also, the guy who said beta-blockers are just for people who won’t fix their lives? That’s not helpful. Some of us have genetic heart conditions. Some of us had heart attacks. Some of us have arrhythmias. We’re not lazy. We’re surviving.
And if you’re on a beta-blocker and you’re feeling better? That’s not numbness. That’s healing.
Just because you don’t understand it doesn’t mean it’s wrong.
Thanks for the post. It’s the kind of clarity we need more of.
Neil Mason
November 8, 2025 AT 08:04As a Canadian who’s been on bisoprolol for 7 years after a heart attack, I just want to say thank you for writing this. I’ve had so many doctors here assume I’m just ‘an anxious guy’ and push me toward SSRIs. But it was the beta-blocker that saved me.
Also, I switched from metoprolol tartrate to succinate and it was like night and day. No more 3pm crashes. No more double-dosing confusion.
And the sexual side effect thing? Yeah, my wife noticed the difference when I switched to nebivolol. We didn’t even talk about it until she said, ‘You’re more present.’
Canada’s healthcare system doesn’t always get it right, but when it does? This is what it looks like.
One thing I wish more people knew: beta-blockers aren’t just for the heart. They’re for the whole person. If you’re feeling off, ask if it’s the drug. Don’t assume it’s you.
And please, for the love of God, don’t stop cold turkey. I almost did once. Bad idea.
Alexa Ara
November 8, 2025 AT 20:27Thank you for saying that. I was scared to bring up the side effects because I thought I was just being dramatic. But you’re right-it’s not me. It’s the drug. I’m switching to nebivolol next week. Fingers crossed.
And to the guy who said we’re just outsourcing our well-being? I get it. But sometimes, medicine isn’t about fixing your life. It’s about giving you the stability to fix it.
I’m on therapy now. I’m eating better. I’m walking every day.
But I still need this pill to keep my heart from screaming.
And that’s okay.