Most people assume that if a drug is approved and prescribed, it’s safe. But your liver doesn’t always see it that way. Every day, thousands of people take medications without knowing they’re putting their liver at risk. Drug-induced liver injury (DILI) isn’t rare-it’s one of the leading causes of sudden liver failure in the U.S., and it often shows up too late to stop the damage. The worst part? You might not feel anything until it’s serious.
What Exactly Is Drug-Induced Liver Injury?
DILI happens when a medication, herbal supplement, or even a vitamin damages your liver. It’s not the same as alcohol-related liver disease or hepatitis. This damage comes from chemicals your body tries to break down-and sometimes, the breakdown process itself turns toxic. The liver handles over 90% of drug metabolism, making it the most vulnerable organ in your body when it comes to medication side effects.
There are two main types: intrinsic and idiosyncratic. Intrinsic DILI is predictable. Take too much acetaminophen, and you’ll likely hurt your liver. That’s why the maximum daily dose is 3 grams for older adults and those with liver issues. Idiosyncratic DILI is the scary kind. It’s unpredictable. You could take the same dose as someone else, and they’re fine-but you end up in the hospital. This type makes up about 75% of all DILI cases.
Top 5 High-Risk Medications You Should Know
Not all drugs are equal when it comes to liver risk. Some are harmless for most people. Others? They’re quietly damaging livers every day.
- Acetaminophen (Tylenol) - It’s the #1 cause of acute liver failure in the U.S., responsible for nearly half of all cases. A single overdose of 7-10 grams can destroy liver cells. Even regular doses over time, especially when mixed with alcohol, can cause slow, silent damage.
- Amoxicillin-clavulanate (Augmentin) - This common antibiotic causes the most frequent case of idiosyncratic DILI. One in every 2,000 to 10,000 people who take it will develop liver injury. Symptoms often appear 1-6 weeks after starting the drug: yellow skin, dark urine, intense itching.
- Valproic acid - Used for epilepsy and bipolar disorder, this drug can cause severe liver damage in children under two, especially if they’re on multiple seizure meds. Fatality rates in these cases hit 10-20%.
- Isoniazid - A tuberculosis drug that’s been around for decades. It causes liver injury in about 1% of users, but that number jumps to 2-3% if you’re over 35. Many patients don’t realize their fatigue and nausea are signs of liver trouble until their ALT levels spike past 1,000.
- Herbal and dietary supplements - These aren’t just harmless teas. Green tea extract, kava, anabolic steroids, and weight-loss products are now responsible for 20% of DILI cases in the U.S.-up from 7% in the early 2010s. Unlike prescription drugs, they’re not tested for liver safety before sale.
Statins, NSAIDs, and antidepressants also show up on the list-but they’re far less likely to cause serious harm. Still, don’t assume they’re safe. Even mild enzyme elevations can be early warning signs.
How Doctors Spot DILI-And Why It’s Often Missed
There’s no single test for DILI. It’s a diagnosis of exclusion. That means your doctor has to rule out everything else: viral hepatitis, autoimmune disease, fatty liver, alcohol use, gallstones. That’s why many patients wait months before getting the right answer.
Doctors use two main tools: blood tests and the RUCAM scoring system. If your ALT (alanine aminotransferase) is more than 3 times the normal level-or your ALP (alkaline phosphatase) is over 2 times normal-that’s a red flag. The pattern tells the story:
- Hepatocellular pattern (ALT >> ALP): Suggests direct cell damage. Seen with acetaminophen, isoniazid.
- Cholestatic pattern (ALP >> ALT): Suggests bile flow blockage. Common with amoxicillin-clavulanate.
Hy’s Law is another critical clue. If your ALT or AST is over 3x normal and your bilirubin is over 2x normal, you have a 10-50% chance of developing acute liver failure. This combination is a medical emergency.
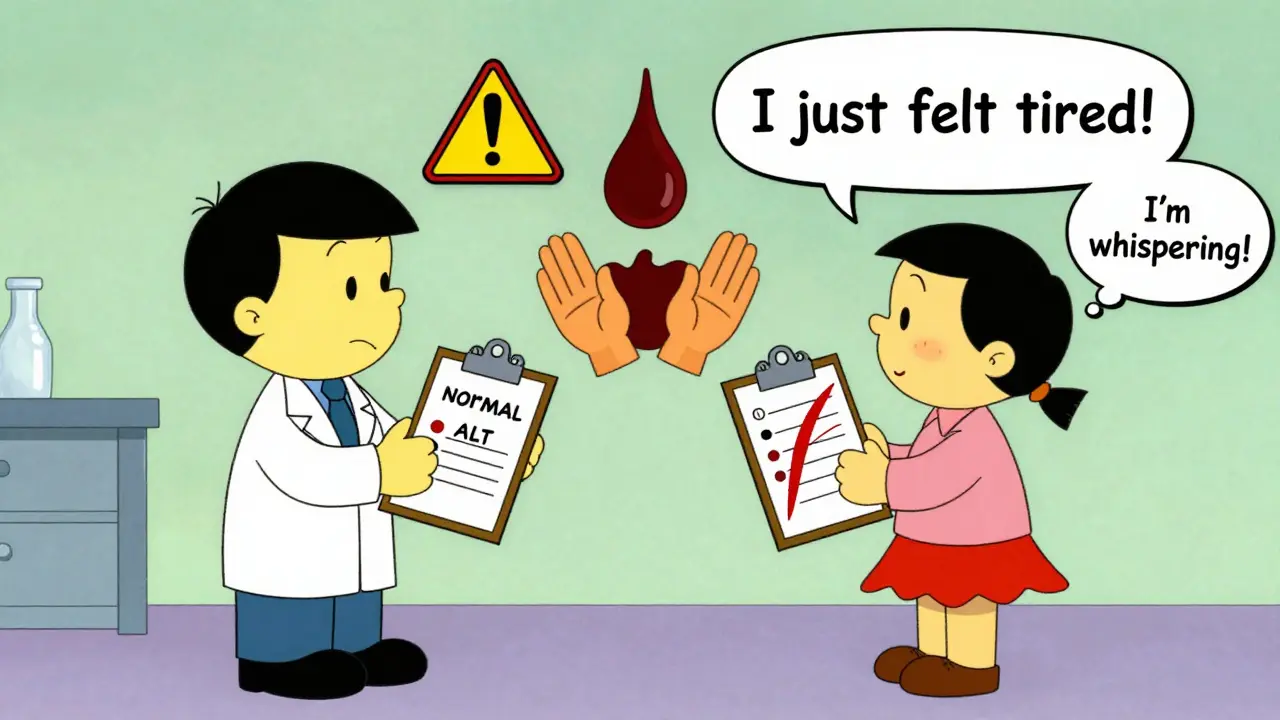
Yet, studies show 68% of DILI patients are misdiagnosed at first. Fatigue? “Stress.” Itchy skin? “Allergy.” Jaundice? “Gallbladder issue.” Too many doctors don’t ask about supplements. Too few check liver enzymes before prescribing high-risk drugs.
Who’s at Highest Risk-and Why
DILI doesn’t pick favorites, but it does favor certain patterns:
- Women - Make up 63% of all cases. Why? Hormonal differences affect how drugs are metabolized.
- People over 55 - Liver function slows with age. Detox pathways get less efficient.
- Those on multiple medications - Drug interactions are a silent killer. A cholesterol pill + an antibiotic + a sleep aid? That combo can overwhelm your liver.
- People with pre-existing liver disease - Even small doses of acetaminophen can be dangerous if your liver is already compromised.
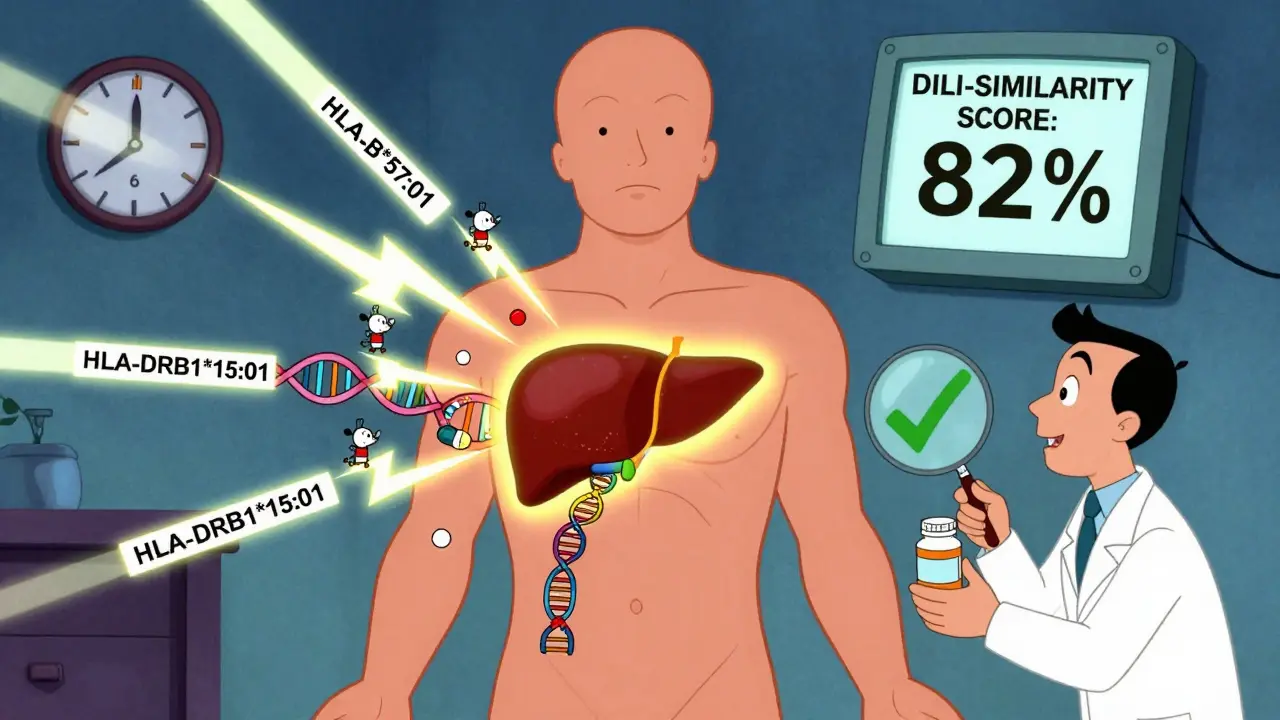
- Genetic factors - Certain gene variants make you more vulnerable. HLA-B*57:01 increases your risk of liver injury from flucloxacillin by 80 times. HLA-DRB1*15:01 raises your risk from amoxicillin-clavulanate by 5.6 times. Genetic testing isn’t routine yet-but it’s coming.
One patient in Scotland took isoniazid for TB and developed jaundice after 10 weeks. His ALT hit 1,200. He didn’t have a history of alcohol use or hepatitis. He was 48. His doctor didn’t test his liver until he turned yellow. It took six months to recover.
How to Monitor Your Liver When Taking High-Risk Drugs
Monitoring isn’t optional for certain drugs. It’s life-saving.
For isoniazid, the CDC recommends:
- Baseline liver test before starting.
- Monthly tests for the first 3 months.
- Then every 3 months after that.
- Stop the drug immediately if ALT rises above 3-5x normal, or if you develop nausea, vomiting, dark urine, or yellow skin.
For valproic acid, especially in children:
- Test liver enzymes before starting.
- Check again at 2 weeks, then monthly for the first 6 months.
- Watch for vomiting, lethargy, or confusion-even if ALT is normal. Valproic acid can cause hyperammonemia without raising enzymes.
For statins, routine monitoring isn’t needed. The risk of severe injury is 1 in 100,000. But you should still know the symptoms: unexplained fatigue, dark urine, pale stools, abdominal pain. If you feel worse after starting a statin, get tested.
For herbal supplements, there’s no official monitoring protocol-because they’re not regulated like drugs. But if you’re taking them, especially for weight loss, joint pain, or anxiety, tell your doctor. Ask for a liver test before and after 6 weeks of use.
What to Do If You Suspect DILI
If you’re on a high-risk medication and feel off, don’t wait. Don’t assume it’s “just a virus.”
- Stop the suspected drug immediately-but only after calling your doctor. Some drugs can’t be stopped cold turkey.
- Get liver function tests right away. Don’t wait for an appointment.
- Bring a full list of everything you take: prescriptions, OTC meds, vitamins, herbs, energy drinks, protein powders.
- Ask your pharmacist to review your meds. They catch interactions doctors miss.
Recovery is possible. About 90% of patients see enzyme levels drop within 1-2 weeks of stopping the drug. Full recovery usually takes 3-6 months. But 12% of people end up with permanent liver damage. And in rare cases, a transplant is the only option.
How Pharmacists Are Preventing DILI Before It Starts
One of the biggest wins in DILI prevention isn’t coming from hospitals-it’s coming from pharmacies. Medication therapy management (MTM) programs, where pharmacists review all your drugs, reduce DILI cases by 23% in patients on five or more medications.
Pharmacists check for:
- Drug-drug interactions (e.g., amoxicillin-clavulanate + valproic acid)
- Overlapping acetaminophen in cold meds
- Herbal supplements that clash with prescriptions
- Age-adjusted dosing
One patient in Edinburgh was about to start a new antibiotic for a sinus infection. Her pharmacist noticed she was also taking green tea extract for “detox” and a seizure medication. The pharmacist flagged the combination as high-risk for DILI. She never took the antibiotic. Her liver stayed healthy.
The Future of DILI Detection
Science is catching up. Researchers are developing tools to predict who’s at risk before they even take a drug.
- DILI-similarity score - A computer model that analyzes a drug’s chemical structure to predict liver risk. It’s 82% accurate.
- Biomarkers - MicroRNA-122 and keratin-18 rise in the blood before ALT does. These could give doctors a 12-24 hour early warning.
- EHR alerts - Electronic health records are now being programmed to flag dangerous drug combos before they’re prescribed. Early trials show they can prevent 15-20% of severe DILI cases.
- Genetic screening - If you’re going on flucloxacillin or amoxicillin-clavulanate, your doctor may soon recommend a simple DNA test to see if you carry the high-risk gene.
The goal isn’t to scare you off meds. It’s to make sure you’re not taking them blind.
Final Takeaways
- Acetaminophen is the #1 cause of sudden liver failure-never exceed 3 grams daily if you’re over 65 or have liver disease.
- Antibiotics like amoxicillin-clavulanate and TB drugs like isoniazid are high-risk. Monitor your liver if you’re on them.
- Herbal supplements aren’t safe just because they’re “natural.” Green tea extract and kava are dangerous.
- Always tell your doctor and pharmacist about every supplement you take.
- Know the warning signs: fatigue, dark urine, yellow skin, itching, nausea. Don’t ignore them.
- Get a liver test before starting high-risk meds-and ask if you need follow-up tests.
Your liver doesn’t scream. It whispers. Listen before it’s too late.


Ron Williams
December 16, 2025 AT 16:05Man, I never realized how many things we pop daily could be quietly wrecking our livers. I take Tylenol for headaches like it’s candy, and now I’m second-guessing every pill. Thanks for laying this out so clearly.
Kitty Price
December 18, 2025 AT 14:23Green tea extract?? 😱 I’ve been taking that ‘detox’ tea for months. Time to stop and get tested. Thanks for the wake-up call! 🙏
Arun ana
December 19, 2025 AT 06:42Same here from India. People think ayurvedic = safe. My uncle took some ‘liver cleanse’ powder and ended up in ICU. No regulation, no testing - just guesswork. We need better awareness here too.
Kayleigh Campbell
December 19, 2025 AT 23:53So let me get this straight - we’re told to avoid sugar, salt, and carbs, but it’s totally fine to chow down on a bottle of acetaminophen like it’s M&Ms? 🤔 The system is designed to keep you sick so you keep buying meds. I’m not mad, I’m just disappointed.
Also, why is it that when a drug kills people, we call it ‘idiosyncratic’? That’s just corporate speak for ‘oops, we didn’t test enough brown people’.
And don’t even get me started on supplements. If your ‘natural’ remedy was FDA-approved, it wouldn’t be sold in a glass jar next to crystals at Whole Foods.
My grandma took isoniazid for TB in ’87. She didn’t even know what ALT stood for. She just trusted the doctor. Turns out, she was one of the lucky ones. Half her friends didn’t make it.
We treat our bodies like disposable gadgets. Plug it in, turn it on, reboot if it glitches. But your liver doesn’t have a reset button. It doesn’t scream. It whispers. And by the time you hear it, you’re already halfway to transplant.
And yet, we still scroll through TikTok detox trends while our enzymes creep up like a slow-motion horror movie.
Pharmacists catching these combos? That’s the real MVP. Doctors are overworked. Nurses are burned out. But the pharmacist? They’re the ones actually reading the labels. We need more of them. Not less.
And if you’re taking statins and feeling like a zombie? Stop blaming your ‘aging’. Get your liver checked. It’s not ‘just fatigue’ - it’s your body screaming in binary.
Also, I’m pretty sure the FDA’s idea of ‘monitoring’ is a Post-It note on a fridge. We need mandatory baseline tests for anything that even smells like it might kill you.
And yes, I’ve told my mom to stop taking that ‘miracle weight loss tea’ she got from her yoga instructor. She’s 68. She’s not detoxing. She’s detoxing her liver.
Listen. Your liver doesn’t care if you’re ‘healthy’. It cares if you’re dumb.
Joanna Ebizie
December 20, 2025 AT 01:28Ugh. Of course the government lets this happen. Big Pharma’s got Congress in their back pocket. They don’t want you to know your Tylenol is basically poison. Just keep buying more.
Elizabeth Bauman
December 20, 2025 AT 08:34Let me be clear - this isn’t about ‘risk’. It’s about betrayal. The FDA is a puppet of foreign drug manufacturers. Why do you think they allow supplements with zero testing? Because they’re outsourcing our health to China and India. And now we’re paying with our livers. This is a national security issue.
Every time someone takes kava or green tea extract, they’re helping fund foreign enemies. This isn’t health advice - it’s treason.
My cousin got liver damage from Augmentin. He’s lucky. He’s American. Imagine if he was in some third-world country with no doctors. We need to ban all non-domestic meds. Period.
And why aren’t we testing everyone’s DNA before they get a prescription? This is basic patriotism. If you’re not willing to get a genetic scan, you don’t deserve to live in this country.
Dylan Smith
December 21, 2025 AT 00:08So I took amoxicillin last month and got really itchy. I thought it was a rash. Now I’m wondering if it was my liver screaming. I didn’t tell my doctor. I just stopped taking it. Should I get tested anyway? I’m scared to ask
Mike Smith
December 21, 2025 AT 07:03Thank you for sharing this critical information with such clarity and care. This is exactly the kind of public health education we desperately need. The liver is an unsung hero - working tirelessly, silently, and without complaint. We owe it more than just a quick dose of pain relief or a trendy supplement.
For those who are now feeling anxious after reading this - please don’t panic. Awareness is the first step toward empowerment. You are not your medication. You are not your liver enzymes. You are someone who is choosing to protect your body, and that is a profound act of self-respect.
Reach out to your pharmacist. Request a baseline liver panel before starting any new regimen. Ask your doctor if genetic screening is appropriate for you. Advocate for yourself - not aggressively, but persistently.
And if you’re a healthcare provider reading this - thank you. You are the frontline defense against silent harm. Keep asking the hard questions. Keep checking the labs. Keep listening to the whispers.
This isn’t fear-mongering. This is foresight. And foresight saves lives.
Aditya Kumar
December 23, 2025 AT 06:35Too much info. I just take what the doctor says.
Colleen Bigelow
December 24, 2025 AT 21:30Of course the government doesn’t regulate supplements. They’re scared of the truth - that real medicine is controlled by global elites who profit from your suffering. Kava and green tea extract? They’re natural weapons against Big Pharma’s synthetic poisons. But they’re also being banned because they’re too effective. They’re exposing the lie that you need a prescription to heal.
And why is acetaminophen still legal? Because it’s cheaper than a liver transplant. The system wants you sick, not healed. The real danger isn’t the drug - it’s the silence. They don’t want you talking about this. That’s why they call it ‘idiosyncratic’. So you’ll blame yourself, not the system.
My cousin took Tylenol for a headache. She woke up in the ICU. They said it was ‘unpredictable’. But I know better. It was a cover-up. The same people who told you vaccines were safe are the ones who approved this poison. Wake up.