Glaucoma Eye Drop Comparison Tool
Select Eye Drops to Compare
Comparison Results
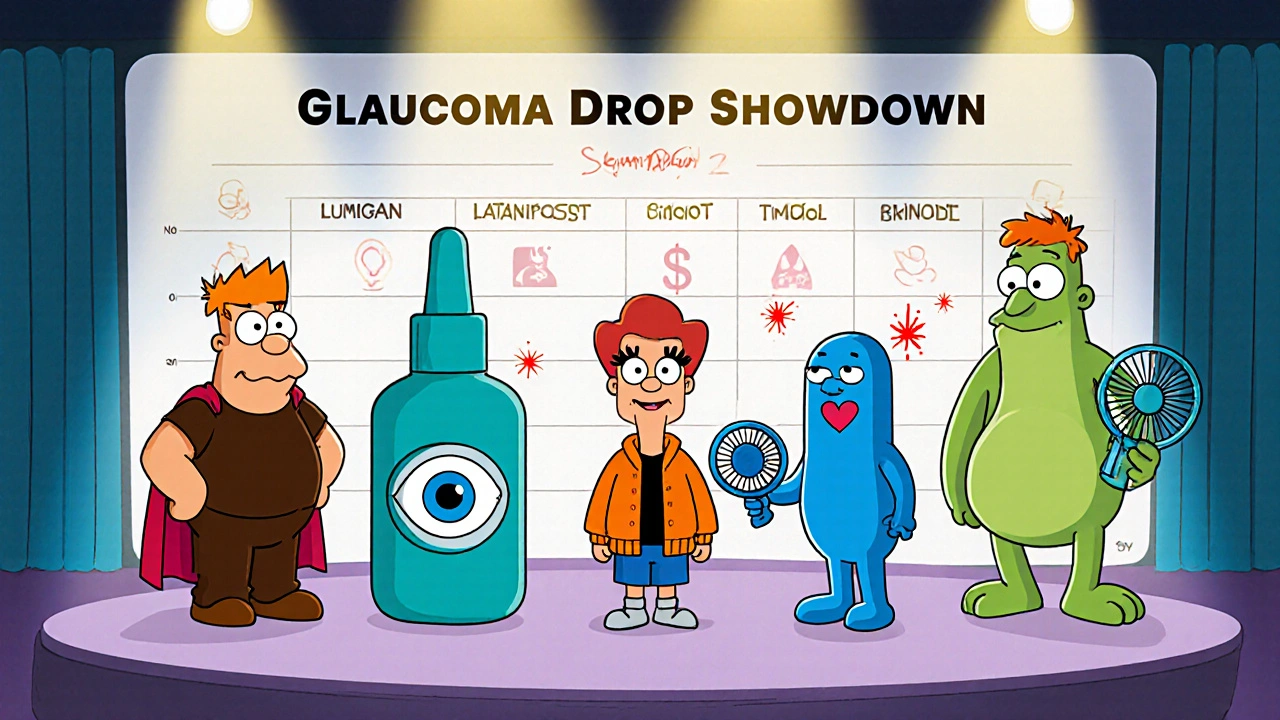
| Metric | Lumigan | Latanoprost | Travoprost | Timolol | Brimonidine |
|---|---|---|---|---|---|
| Typical IOP Reduction | 25-30% | 22-28% | 24-30% | 15-20% | 18-25% |
| Key Side Effects | Darkening iris, eyelash growth, redness | Mild redness, occasional iris darkening | Conjunctival hyperemia, brownish eyelash change | Bronchospasm risk, bradycardia, dry eye | Allergic conjunctivitis, fatigue, dry mouth |
| Cost (UK) | £45-£55 | £12-£20 (generic) | £30-£38 | £5-£10 | £15-£22 |
| Best For | Patients needing maximum IOP reduction | Cost-conscious patients with no color change concerns | Patients needing strong efficacy with less pigmentation | Patients without respiratory issues needing moderate reduction | Patients wanting lower IOP with minimal hyperemia |
When it comes to managing primary open‑angle glaucoma, picking the right eye drop can feel like a high‑stakes gamble. Lumigan (Bimatoprost) is a prostaglandin analog designed to lower intra‑ocular pressure (IOP) by improving aqueous humor outflow. But dozens of other drops sit on pharmacy shelves-some brand‑name, some generic-each with its own profile of efficacy, side‑effects, and cost. This guide breaks down Lumigan and its most common alternatives, so you can see exactly where the strengths and trade‑offs lie.
How Lumigan Works
Lumigan belongs to the prostaglandin‑F2α (PGF2α) class. After instillation, bimatoprost binds to FP receptors in the ciliary muscle, opening the trabecular meshwork and expanding the uveoscleral pathway. The result is a 25‑30% reduction in IOP for most patients, an effect that kicks in within 24 hours and peaks at about eight weeks of consistent use.
Key Attributes of Lumigan
- Dosage: One drop in the affected eye(s) once daily, preferably in the evening.
- Typical IOP reduction: 25‑30% for treatment‑naïve eyes; up to 35% when combined with a carbonic anhydrase inhibitor.
- Common side‑effects: Darkening of the iris, eyelash growth, conjunctival hyperemia, and occasional ocular irritation.
- Contra‑indications: Active ocular inflammation, known hypersensitivity to bimatoprost or any component of the formulation.
Because the pigment‑darkening effect can be permanent, many clinicians reserve Lumigan for patients who do not have light‑colored irises or who are comfortable with the cosmetic change.
Alternative Prostaglandin Analogs
The prostaglandin family includes several other drops that share a similar mechanism but differ in potency, dosing convenience, and side‑effect profile.
Latanoprost is a prostaglandin F‑type analog that reduces IOP by increasing uveoscleral outflow. It’s been on the market since 1996 and is often the first‑line generic choice.
Travoprost is a PGF2α analog with a slightly higher affinity for the FP receptor compared with latanoprost. Travoprost is available both as a preservative‑free formulation and in a standard bottle.
Timolol is a non‑selective beta‑blocker that lowers IOP by reducing aqueous humor production. Although not a prostaglandin, it’s frequently combined with prostaglandins in fixed‑dose products.
Brimonidine is an α‑2 adrenergic agonist that both decreases aqueous production and increases uveoscleral outflow. It’s useful when a modest IOP drop is needed without the hyperemia often seen with prostaglandins.
Side‑Effect Snapshot Across Options
| Medication | Typical IOP Reduction | Key Adverse Events | Cost (UK, per pack) |
|---|---|---|---|
| Lumigan (Bimatoprost) | 25‑30% | Darkening iris, eyelash growth, redness | £45‑£55 |
| Latanoprost | 22‑28% | Mild redness, occasional iris darkening (less common) | £12‑£20 (generic) |
| Travoprost | 24‑30% | Conjunctival hyperemia, brownish eyelash change | £30‑£38 |
| Timolol (monotherapy) | 15‑20% | Bronchospasm risk, bradycardia, dry eye | £5‑£10 |
| Brimonidine | 18‑25% | Allergic conjunctivitis, fatigue, dry mouth | £15‑£22 |
Choosing Between Lumigan and Its Peers
Clinical decision‑making often hinges on three pillars: efficacy, tolerability, and patient‑specific factors.
- Efficacy First: If you need the steepest IOP drop-say, in a patient with advanced optic‑nerve damage-Lumigan or Travoprost usually edge out latanoprost.
- Tolerability Concerns: Patients with light‑colored irises who dislike cosmetic changes may prefer latanoprost, which has a lower incidence of permanent pigmentation.
- Comorbidities: Anyone with asthma or severe COPD should avoid timolol. Brimonidine can cause fatigue, so it’s less ideal for shift workers.
In practice, many eye‑care professionals start with a generic prostaglandin (latanoprost) because of its low cost and solid efficacy. If the IOP target isn’t met after 4‑6 weeks, they step up to Lumigan or Travoprost.
Cost, Availability, and NHS Coverage
The UK National Health Service typically lists latanoprost as the default first‑line agent on its prescription formularies. Lumigan, being a branded product, often requires a special authority request unless the patient qualifies for the NHS “high‑cost” exception (e.g., intolerance to latanoprost). Timolol remains the cheapest option, especially as a generic, but its lower efficacy means it’s usually a second‑line adjunct rather than a stand‑alone.
Practical Checklist for Clinicians and Patients
- Confirm diagnosis of primary open‑angle glaucoma with visual‑field testing.
- Measure baseline IOP three times on different days.
- Start with latanoprost (generic) unless contraindicated.
- Re‑measure IOP after 4‑6 weeks; if reduction <20%, discuss switching to Lumigan or Travoprost.
- Ask about eye colour and cosmetic preferences; explain potential iris darkening.
- Screen for respiratory issues before prescribing timolol.
- Review cost and NHS formulary status; consider patient assistance programs for branded drops.
- Schedule follow‑up at 3 months, then every 6-12 months for optic‑nerve monitoring.
Frequently Asked Questions
Can Lumigan cause permanent eye color change?
Yes. The brown pigment can become permanent, especially in patients with light‑colored irises. Discuss this risk before starting therapy.
How quickly does Lumigan start lowering IOP?
A measurable drop appears within 24 hours, with the peak effect around 8 weeks of consistent use.
Is it safe to use Lumigan with other glaucoma drops?
Combining a prostaglandin (like Lumigan) with a carbonic anhydrase inhibitor or beta‑blocker is common and can provide additive IOP reduction.
What are the main reasons to choose latanoprost over Lumigan?
Lower cost, lower risk of permanent iris darkening, and a solid efficacy record make latanoprost the go‑to first‑line agent for many patients.
Are there any drug interactions with Lumigan?
No major systemic interactions are known, but topical NSAIDs may increase ocular irritation. Always inform the ophthalmologist about all eye drops you are using.
Choosing the optimal glaucoma drop boils down to balancing how much pressure you need to lower, how the patient tolerates side‑effects, and what the NHS will cover. Lumigan remains a powerful tool in the arsenal-especially when a deeper IOP cut is required-but it isn’t the only game‑changer. By comparing its profile against latanoprost, travoprost, timolol, and brimonidine, you can tailor the regimen to each individual’s eyes and lifestyle.

erica fenty
October 21, 2025 AT 15:07The pharmacodynamics of bimatoprost involve FP‑receptor agonism, upregulation of matrix metalloproteinases, and consequent remodeling of the trabecular meshwork, thereby augmenting uveoscleral outflow; this cascade yields a robust 25‑30% IOP reduction, as documented in multiple Phase III trials, and is dose‑independent beyond the standard 0.03% formulation.
Ericka Suarez
November 7, 2025 AT 08:20We dont need these foreign eye drops to control our vision, the American way is the only way! If they try to push Lumigan on us it's a conspiracy to drain our wallets.
parbat parbatzapada
November 24, 2025 AT 17:00they say it's just a prostaglandin but i heard the pharma guys mixed some micro‑chips in the bottle, just in case they can track our pressure readings, keep an eye out.
Casey Cloud
December 13, 2025 AT 05:26Start with baseline measurement before initiating any prostaglandin therapy.
Take three IOP readings on different days to establish variability.
Choose latanoprost as first‑line if cost is a concern and there are no contraindications.
If the IOP reduction after six weeks is less than 20% consider switching to bimatoprost.
Check for ocular surface irritation after each drop change.
Document any change in iris colour, especially in patients with light‑coloured eyes.
Avoid bimatoprost in patients with active uveitis or known hypersensitivity.
For patients with respiratory disease steer clear of timolol due to beta‑blockade risk.
Combine a prostaglandin with a carbonic anhydrase inhibitor when monotherapy fails to meet target pressure.
Watch for hyperemia; if it becomes bothersome consider travoprost preservative‑free formulation.
Educate patients on proper drop instillation to prevent systemic absorption.
Schedule follow‑up visual field testing every 6–12 months to monitor progression.
Discuss the cosmetic impact of darkened lashes and iris with the patient early in therapy.
If adherence is an issue, a fixed‑dose combination may simplify the regimen.
Finally, review NHS formulary guidelines to ensure the prescribed agent is authorized for reimbursement.
Rachel Valderrama
December 31, 2025 AT 17:53Oh great, another eye drop that’ll turn my eyes into a costume.
Brandy Eichberger
January 19, 2026 AT 06:20While the data clearly favours bimatoprost for maximal pressure reduction, I’d still recommend starting with the more economical latanoprost-think of it as a sensible apprenticeship before graduating to the premium formulation.
Eli Soler Caralt
February 6, 2026 AT 18:46In the grand tapestry of ocular therapeutics, each drop is but a brushstroke on the canvas of vision; bimatoprost paints with bold hues of efficacy, yet we must contemplate the ethical palette of cost and cosmetic consequence 🤔✨