Statins & Rhabdomyolysis Risk Calculator
Understand Your Risk
This tool estimates your risk of rhabdomyolysis based on factors discussed in the article. Remember: This is not medical advice.
Enter Your Details
Most people taking statins never experience serious problems. But for a tiny fraction, a quiet, dangerous process can start in their muscles - one that, if missed, can lead to kidney failure or even death. This is rhabdomyolysis, a condition where muscle tissue breaks down rapidly, spilling toxic proteins into the bloodstream. It’s rare - only about 1.5 to 5 cases per 100,000 people taking statins each year - but when it happens, it doesn’t wait for a second opinion.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis isn’t just sore muscles. It’s the literal breakdown of skeletal muscle cells. When these cells die, they release a protein called myoglobin into the blood. Myoglobin is harmless in muscle, but it’s toxic to the kidneys. If too much gets filtered through, it can clog the tiny tubes inside the kidneys, leading to acute kidney injury. In severe cases, patients need dialysis. Some don’t survive. The signs aren’t always obvious at first. You might feel more tired than usual. Your legs might ache like you’ve done a tough workout - even if you didn’t move much. Some people notice dark, tea-colored urine. That’s a red flag. It means myoglobin is being flushed out. Others feel weak, especially when climbing stairs or getting up from a chair. These symptoms often show up within the first three months of starting a statin, or after increasing the dose.Why Do Statins Cause This?
Statins work by blocking an enzyme called HMG-CoA reductase. That’s how they lower cholesterol. But that same enzyme is also needed to make other important molecules in your body - including coenzyme Q10 (CoQ10) and certain fats that help keep muscle cell membranes stable. One theory is that statins drain your muscles of CoQ10, a compound your body uses to produce energy. Without enough, muscle cells struggle to function and start breaking down. Another idea is that statins trigger a cellular cleanup system called the ubiquitin-proteasome pathway, which normally removes damaged proteins - but when overactivated, it starts chewing up healthy muscle tissue. There’s also evidence that statins can make muscle cell membranes more fragile. Think of it like a balloon filled with too much air. If you stretch it too far - say, during a hike or a long walk - it pops. In people taking statins, especially lipophilic ones like simvastatin or lovastatin, the membrane might be more prone to tearing under physical stress. It’s not just one thing. Experts agree: multiple pathways are likely at play. That’s why some people get muscle pain on low doses, while others take high doses for years with no issues.Not All Statins Are the Same
Your risk depends heavily on which statin you’re taking and how much. Simvastatin, especially at 80 mg, carries the highest risk. In fact, the FDA warned in 2011 that the 80 mg dose should no longer be prescribed for new patients because it raised the risk of muscle damage by more than 10 times compared to lower doses. Pravastatin and fluvastatin are much safer in this regard. Rosuvastatin and atorvastatin fall in the middle. Why the difference? It comes down to how the body processes them. Statins like simvastatin, lovastatin, and atorvastatin are broken down by a liver enzyme called CYP3A4. If you’re taking another drug that blocks this enzyme - like the antibiotic clarithromycin or the antifungal itraconazole - your statin levels can spike dangerously high. One case report showed clarithromycin increasing simvastatin levels by 10 times. Even without drugs, your genes matter. A common variation in the SLCO1B1 gene - found in about 1 in 10 people - makes your liver less efficient at clearing statins from your blood. People with two copies of this gene variant have up to a 4.5 times higher risk of muscle damage. Testing for this variant is available, though it’s not routine yet.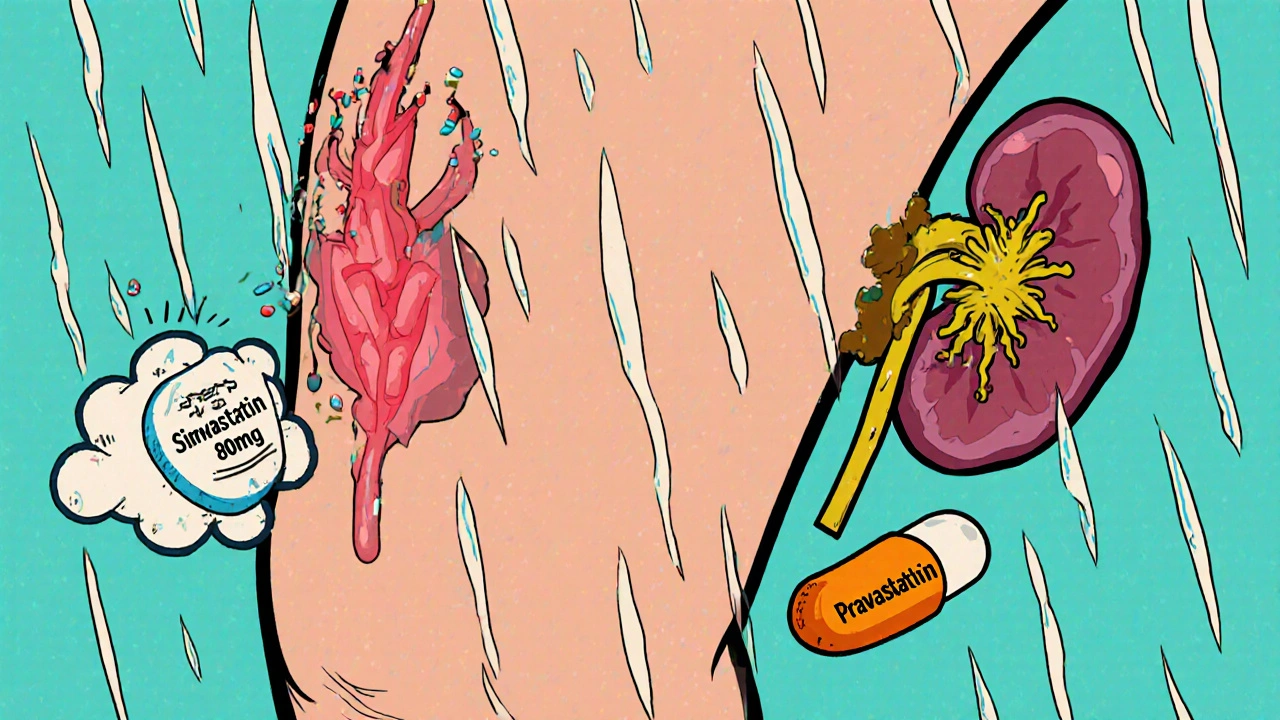
Who’s Most at Risk?
Age is a big factor. About 78% of rhabdomyolysis cases linked to statins happen in people over 65. Women are more commonly affected than men - 62% of reported cases. That’s likely because older women often take more medications, have lower muscle mass, and may be on higher statin doses due to heart disease risk. Other risk boosters include:- High-dose statins (especially simvastatin 80 mg)
- Combining statins with drugs that interfere with liver metabolism
- Having kidney disease or hypothyroidism
- Being physically active - especially doing eccentric exercises like downhill walking or lowering weights
- Genetic factors like the SLCO1B1 variant
What Should You Do If You Have Muscle Pain?
Not every ache means trouble. About 5% to 29% of statin users report mild muscle discomfort - often called statin-associated muscle symptoms (SAMS). But if the pain is new, deep, persistent, or worse after activity, don’t ignore it. Your doctor should check your creatine kinase (CK) levels. This enzyme leaks into the blood when muscles break down. A level more than 10 times the normal upper limit is a clear signal to stop the statin. If your CK is above 10,000 IU/L and you have dark urine or swelling, you need urgent care. Dehydration can make kidney damage worse, so drink water - but don’t wait to get to the hospital if you’re feeling unwell. Physical therapists often use a simple checklist: muscle weakness, pain that doesn’t improve with rest, and fatigue that feels different from normal tiredness. If all three are present, it’s time to talk to your doctor.
What Happens After Rhabdomyolysis?
If you’ve had rhabdomyolysis from a statin, you should never take that same statin again. But that doesn’t mean you can’t manage your cholesterol. Some patients can try a different statin - like pravastatin or rosuvastatin - at a low dose, with close monitoring. Others may switch to non-statin options like ezetimibe or PCSK9 inhibitors. But here’s the catch: PCSK9 inhibitors cost about $5,850 a year. Most insurance won’t cover them unless you’ve tried and failed multiple statins. There’s good news, though. A 2023 study found that 78% of people who thought they were “statin intolerant” could actually tolerate a different statin or a lower dose after proper guidance. Many of the symptoms people blame on statins are actually the nocebo effect - where expecting side effects makes you more likely to feel them.Can You Prevent This?
Yes - with awareness and smart choices.- Don’t start high-dose statins without a clear reason. Lower doses often work just as well for prevention.
- Tell your doctor about every medication and supplement you take - including over-the-counter painkillers and herbal products.
- Avoid grapefruit juice if you’re on simvastatin, lovastatin, or atorvastatin. It interferes with how your body breaks them down.
- Don’t suddenly start intense workouts. Ease into exercise, especially if you’re new to it.
- Know your family history. If a close relative had muscle problems on statins, mention it.
- Get your CK checked if you feel unusual muscle pain, especially after starting or increasing your statin dose.
The Bigger Picture: Benefits vs. Risks
Let’s be clear: statins save lives. In the U.S. alone, they prevent about 500,000 heart attacks and strokes every year. For someone with a history of heart disease, diabetes, or high LDL cholesterol, the benefits of taking a statin far outweigh the tiny risk of rhabdomyolysis. But for healthy people taking statins for primary prevention - especially older adults with borderline cholesterol - the risk-benefit balance gets trickier. That’s why personalized medicine is becoming more important. Genetic testing, better biomarkers, and smarter dosing are helping doctors match the right drug to the right person. A 2023 study identified 17 blood proteins that predict statin muscle damage with 89% accuracy. Soon, we might be able to test for this risk before even starting a statin. For now, the message is simple: don’t panic. Statins are safe for most people. But if you feel something off - especially muscle pain that doesn’t go away - speak up. Early detection saves kidneys. And lives.Can statins cause muscle pain without rhabdomyolysis?
Yes. Mild muscle pain, cramps, or weakness - known as statin-associated muscle symptoms (SAMS) - affect 5% to 29% of users. This is not rhabdomyolysis. It’s usually not dangerous, but it can be uncomfortable enough to make people stop taking their medication. If the pain is mild and doesn’t worsen with activity, your doctor may lower the dose or switch you to a different statin instead of stopping completely.
Is rhabdomyolysis reversible?
Yes, if caught early. Stopping the statin and getting proper hydration and medical care can fully reverse muscle damage and prevent kidney injury. But if treatment is delayed and kidney failure develops, the damage can be permanent. In rare cases, it can be fatal. That’s why recognizing symptoms quickly is critical.
Do I need genetic testing before taking statins?
Not routinely. But if you’ve had muscle pain on a statin before, or if you’re starting high-dose simvastatin and have other risk factors (like age over 65 or kidney disease), your doctor may consider testing for the SLCO1B1 gene variant. The test costs around $250 and can help guide safer dosing - especially if you’re a homozygous carrier, who should avoid doses above 20 mg of simvastatin.
Can I take CoQ10 supplements to prevent statin muscle pain?
Some people report feeling better on CoQ10 supplements, but clinical trials haven’t proven they prevent rhabdomyolysis or reliably reduce muscle pain. The theory makes sense - statins lower CoQ10 - but the evidence is mixed. It’s not harmful to try, but don’t assume it will solve the problem. Always talk to your doctor before starting supplements.
What should I do if I notice dark urine while on a statin?
Seek medical attention immediately. Dark, tea-colored urine is a sign of myoglobin in your blood - a hallmark of rhabdomyolysis. Don’t wait. Go to an urgent care center or emergency room. Early treatment with fluids and monitoring can prevent kidney damage. Bring your statin bottle and a list of all your medications.

Peter Stephen .O
November 16, 2025 AT 09:41Man I never realized statins could mess with your muscles like this. I was on simvastatin for two years and thought my leg cramps were just from biking too hard. Turns out I was lucky I didn’t end up in the hospital. Seriously, if you’re on these meds and feel weird muscle fatigue, don’t brush it off. Your body’s screaming for attention.
Georgia Green
November 18, 2025 AT 05:15My dr told me to take CoQ10 and it helped my cramps. Not sure if it was placebo or not but i felt better. also avoid grapefruit. i learned that the hard way.
Rob Goldstein
November 18, 2025 AT 21:50As a clinical pharmacist, I’ve seen this too many times. Rhabdomyolysis is rare but when it hits, it hits hard. The key is early CK testing - don’t wait for dark urine. Many patients dismiss muscle pain as aging or overexertion. But if it’s new, persistent, and worse with activity, it’s not normal. And yes, pravastatin is the safest bet for high-risk folks. Genetic testing? Not routine, but if you’ve had muscle issues before, it’s worth asking for.
George Gaitara
November 19, 2025 AT 03:00Wow, so statins are basically slow poison for your muscles? And the FDA knew about this since 2011 but still lets doctors prescribe 80mg simvastatin to people who don’t even need it? This is pharmaceutical greed disguised as medicine. You think your cholesterol is the enemy? Nah. The real enemy is the system that profits from your fear.
Andrew Cairney
November 21, 2025 AT 02:55LOL the nocebo effect? So if I feel muscle pain it’s all in my head? 😂 Meanwhile my cousin went from walking fine to needing a cane after statins and they told him it was ‘just anxiety’. Then he got CK levels checked - 18,000 IU/L. Kidney failure. Now he’s on dialysis. Thanks for the ‘nocebo’ theory, bro. Real helpful.
Also, why are they still selling simvastatin 80mg? It’s basically a death sentence for anyone over 60. Someone’s making bank on this.
And don’t even get me started on PCSK9 inhibitors - $6k a year? Who’s gonna pay for that? Not me. Not my mom. Not anyone without a trust fund. 😒
Kathy Grant
November 22, 2025 AT 18:37I’ve been thinking a lot about this lately - how we treat our bodies like machines that should just keep running, no matter the cost. We take pills to fix symptoms without asking why the system broke down in the first place. Statins lower cholesterol, sure - but what if the real issue is inflammation? Or insulin resistance? Or stress? We’re so quick to slap a chemical on the problem instead of looking at the whole picture. Maybe the real danger isn’t the statin… it’s how little we listen to our bodies until it’s too late.
I’m not saying don’t take them. I’m saying - be curious. Be gentle. Ask questions. And if your muscles start whispering, don’t shout over them.
Christina Abellar
November 22, 2025 AT 23:01Dark urine = go to ER. No exceptions.
vinod mali
November 24, 2025 AT 20:19i am from india and many people here take statins without knowing risks. doctors dont explain well. i told my uncle to get ck test after he had leg pain - he did, and they found it was statin. switched to pravastatin and now he’s fine. just talk to your doctor, dont ignore.
Robert Merril
November 26, 2025 AT 20:03So let me get this straight - you’re telling me I can’t eat grapefruit with my statin but I can drink 3 energy drinks a day and no one cares? 🤡
Also CoQ10 supplements? That’s like putting duct tape on a leaking submarine. And why is this even a debate? If a drug causes your muscles to melt, maybe we should just… not give it to people?
Also who the hell wrote this article? It’s like a pharmaceutical ad disguised as a public service announcement. ‘Statins save lives!’ Yeah, and cigarettes used to be ‘doctor recommended’ too.
Dave Feland
November 28, 2025 AT 07:24Did you know that the statin industry is funded by the same people who pushed trans fats as ‘heart healthy’? This isn’t medicine - it’s a controlled population reduction program disguised as prevention. They don’t want you healthy. They want you dependent. And that genetic test? It’s not for your benefit. It’s to make sure you’re locked into the system. The real risk isn’t rhabdomyolysis - it’s blind trust in institutions.
Jennie Zhu
November 29, 2025 AT 12:58It is imperative to underscore that while the incidence of statin-induced rhabdomyolysis remains exceedingly low, the clinical consequences are profound and potentially irreversible. Elevated creatine kinase levels exceeding tenfold the upper limit of normal constitute a clear diagnostic threshold, necessitating immediate discontinuation of the offending agent and aggressive hydration. Furthermore, the pharmacokinetic interactions mediated by the CYP3A4 isoenzyme pathway warrant meticulous medication reconciliation, particularly in polypharmacy patients. The SLCO1B1 polymorphism, while not routinely screened, represents a validated pharmacogenomic biomarker that may significantly mitigate risk in susceptible subpopulations.
Ashley Unknown
November 29, 2025 AT 17:46Okay so let me get this straight - statins are causing muscle breakdown, kidney failure, and death, and they’re telling us it’s ‘rare’? But how rare is it really? I bet they’re hiding the numbers. And why is it always older women? Because they’re the ones being prescribed these drugs like candy while the men get to keep their testicles and their freedom? This is medical misogyny. And don’t even get me started on how they push PCSK9 inhibitors at $6k a year while ignoring the real cause - processed food, corporate greed, and the pharmaceutical cartel that owns Congress. I’ve been reading about this for months. They’re poisoning us slowly and calling it ‘preventive care’. Wake up.
My aunt died from this. They told her it was ‘just old age’. She was 67. She never even had a heart attack. She just took her statin and one day her legs wouldn’t move. They didn’t test her CK until it was too late. Now I don’t trust doctors. I don’t trust pills. I don’t trust the system. And you shouldn’t either.
Roberta Colombin
November 30, 2025 AT 20:32Thank you for sharing this with such care. Many people feel alone when they experience side effects from medications. It’s important to remember that your experience matters - even if it’s rare. If you’re worried, talk to your doctor. And if they don’t listen, find someone who will. You deserve to be heard. And you’re not crazy for wanting to feel well.
Noel Molina Mattinez
December 1, 2025 AT 13:15Statins are just a scam to make people buy more drugs. I stopped mine and my cholesterol went up but I feel 10x better. No muscle pain no fatigue no nothing. The real problem is sugar and processed food not cholesterol. They just want you hooked on pills. I’m not taking any more.